|
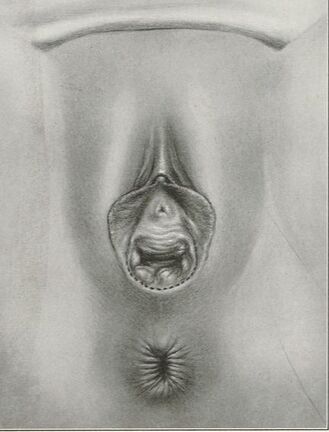
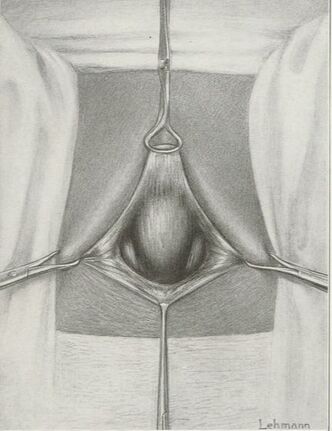
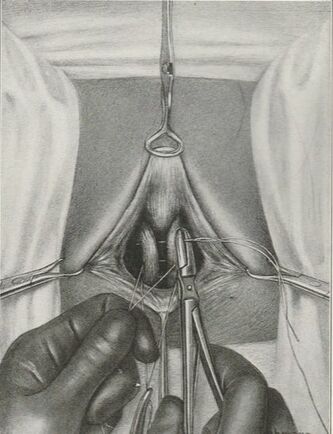
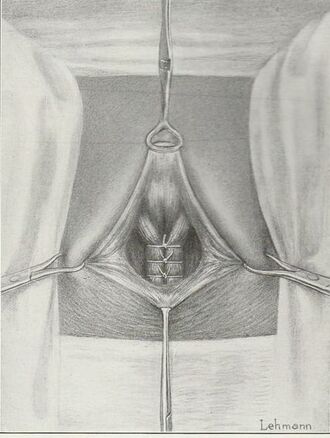
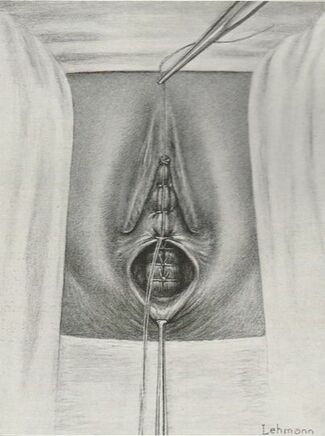
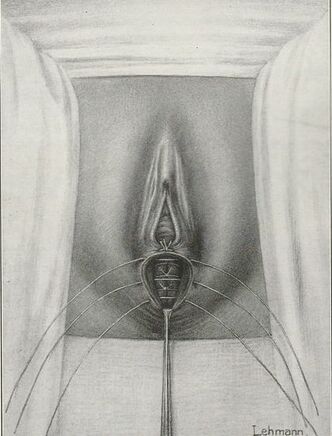
Tranexamic acid is the latest adjunct in cosmetic surgery for the reduction of bleeding, bruising, and postoperative swelling. Popular in the oral form (Lysteda) as a treatment for heavy menses since the 1980s, and the intravenous form (Cyklokapron) in cardiovascular and orthopedic surgery for the control of surgical hemorrhage for decades, it has also been used effectively by direct application to the surgical field by irrigation, soaked pledgets and tissue injection in hair transplantation and various aesthetic procedures of the face, breasts, and abdomen including liposuction. We have been using topical tranexamic acid in blephoroplasty, breast augmentation, abdominoplasty, liposuction, and abdominoplasty, and vaginoplasty for the past year with similar positive findings to those of recent authors. There is no precedent in vaginoplasty to the best of our knowledge. How we use tranexamic acid in cosmetic gynecologyA wide range of effective dosages for topical tranexamic acid is reported in the literature. Our most common application is in liposuction and the dosage we have been using for this procedure is 500mg tranexamic acid per liter of tumescent local anesthesia (TLA). We have used the same dose for all other applications including vaginoplasty. The method of topical application has been direct tissue injection at the time of local anesthesia infiltration and TLA-soaked surgical sponges. In the vaginoplasty example above, the right sided puborectalis muscle (medial border inked) is about to be injected with Tranexamic-TLA in preparation for levatorplasty. A midline pleated rectocele repair has been completed and the suture line is obvious centrally. Notice the excellent hemostasis of the entire field despite the extent of the dissection. Same operation after completion of a three-layer continuous levatorplasty. There is no bleeding from the puborectalis suture line. This means less postoperative swelling, inflammation and discomfort. Same operation at final stage (perineal reconstruction) showing hemostasis of the deep transverse perineal muscles (inked), superfical perineal muscles, and bulbocavernosus. The surgical sponge in the vaginal canal is serving as a temporary scaffolding for contour adjustment purposes, not for hemostasis. What precautions need to be taken when using tranexamic acid?Tranexamic acid is excreted through the kidneys. Patients must have normal renal function. Also, the concomitant use of oral contraceptives or a history of thromboembolic disease are contraindications to the use of tranexamic acid. The use of tranexamic acid has not been found to increase the surgical risk of thrombembolic disease. How does tranexamic acid work?This post was written as a practice pearl, recipe-style. You can delve into the mechanisms of action of tranexamic acid here. In brief, tranexamic acid keeps newly-formed blood clots from being broken down (fibrinolysis) by inhibiting plasmin.
5 Comments
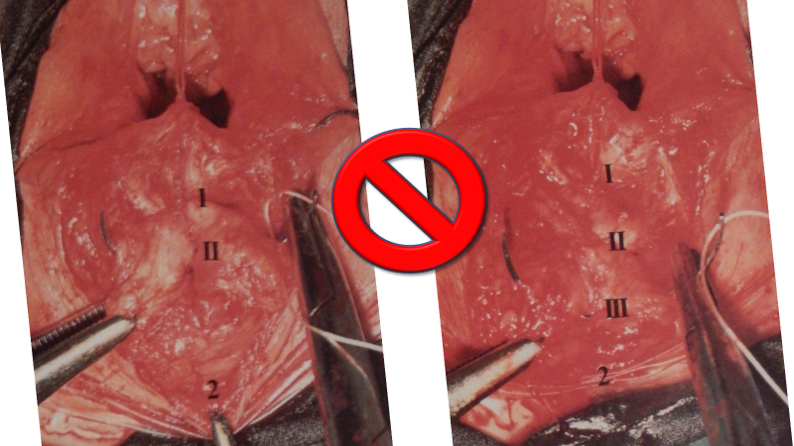
They say levatorplasty is wrong. They say levatorplasty causes painful sex. They point to ancient literature and say, "there's the proof". They write new articles referencing the ancient literature and say, "look, there's more proof - it's in the references". I say they're wrong. Not about the accuracy of what they referenced. I've read the ancient literature, the modern literature, and everything in between. I've been performing levatorplasties for over two decades. My patients aren't experiencing the painful sex that my contemporaries have referenced and the Ancients have described. What's going on here? A review of the history of levatorplasty indicates clearly that their levatorplasty and my levatorplasty are not the same. A review of the ancient "proof" of levatorplasty-induced sexual pain (dyspareunia) reveals that these procedures were overaggressive in certain respects and incomplete in others. For the uninitiated, levatorplasty or more accurately, anterior levatorplasty is the practice of suturing the medial-most portion of the levator ani fibers (a section of the muscle called the puborectalis) immediately proximal to the anal sphincters across the midline and advancing this plication proximally, This is usually done through a perineal incision extended to the posterior vaginal wall. The practice of levatorplasty was introduced by Robert Ziegenspeck of Germany in 1900. To understand the problem with the "wrong" techniques of levatorplasty, we need to go back one hundred years ago and examine the work of Arnold Sturmdorf: In 1919, the influential and innovative Arnold Sturmdorf of New York, published and illustrated his technique of levatorplasty in his book, Gynoplastic Technology. His approach to muscle plication was incorporated by almost all techniques that followed. Sturmdorf's levator "myorrhaphy" begins with a horizontal incision at the introitus and a peeling of the posterior vaginal wall cephalad without additional incision of the flap. This exposes the rectocele defect centrally and the medial borders of the levator ani (puborectalis). No tissue is excised. No suturing is done on the rectocele bulge. Sturmdorf describes the plication, "The sutures passed entirely round (not through) the muscle-shanks, encircling them so as to secrure the broadest possible side-to-side surface contact under the vaginal floor." The procedure concludes with a longitudinal closure of the horizontal skin incision. No skin is excised. It is clear that the levator plication sutures are extremely broad and deep. The complete "encirclement" of these muscles and ligation places extreme tension on a large mass of tissue. This will undoubtedly cause ischemia and ischemia will cause significant discomfort in the short term. In the long term, chronic tension on the muscle tissue will predispose to myalgia and traction pain on nerve fibers. The absence of an independent repair of the rectocele bulge creates two problems. First, it places all of the tension of subsequent bowel movements directly onto a single plane of tissue placing additional stress centrally. It would surprise no one that this type of levatorplasty would create pain with sex or any activity that stresses the muscle tissue. Second, it leaves the low-pressure tissue of the rectocele hernia floating, in essence, and free to float cephalad beyond the plication zone and recur later. The most recent of the oft-quoted articles on painful levatorplasty articles was published by Kahn and Stanton in 1997 (BJOG.1997;104:82-86.). They looked retrospectively at 209 British women treated for rectocele using Stanton's mid-century levatorplasty-only method. Painful sex or anatomical difficulty with sex was found in 27 percent, although 18 percent had problems beforehand. Stanton stated that his levatorplasty technique was identical to that of his British colleagues, Lees and Singer (pictured above). The huge needle bites through a large mass of levator muscle tissue indicate an aggressive high-tension approach. The photos also reveal that the rectocele itself is not sutured. Like that of Sturmdorf, this method provokes tension-related issues. In their discussion, Kahn and Stanton opine that dyspareunia is caused by levatorplasty because of "pressure atrophy of the included muscle fibers and subsequent scarring." citing references from the 1920s, but no data (Goff. Surg Gynecol Obstet. 1928;46:855-866). So where does this historical analysis lead us? First, we see that taking huge bites of the levator ani muscle and forcing them together under high tension creates problems. Second, we see that using a single layer of muscle tissue as the only repair for a rectocele creates problems. Third, we see that quoting articles that quote articles doesn't provide data directly and that opinions in the discussion section of published articles aren't exactly the same thing as evidence and might distort the impression of the literature for those who fail to dig a little deeper. I stated that my levatorplasty is not the same as "their" levatorplasty. What's the difference?
It doesn't require huge bites of muscle tissue. It doesn't involve high tension. And it doesn't take place withouit the support of a sturdy rectocele repair underneath to take the tension and stress off the sensitive muscle tissue. Two decades. No problems. No kidding. Would you like to learn more? |
AuthorMarco A. Pelosi, III, MD, is a cosmetic gynecologist, surgeon, lecturer & cofounder of the ISCG. You may contact him directly at [email protected] Archives
April 2020
Categories
All
|
We are ISCG |
Get to Know Us |
Stay Connected |








 RSS Feed
RSS Feed
