|
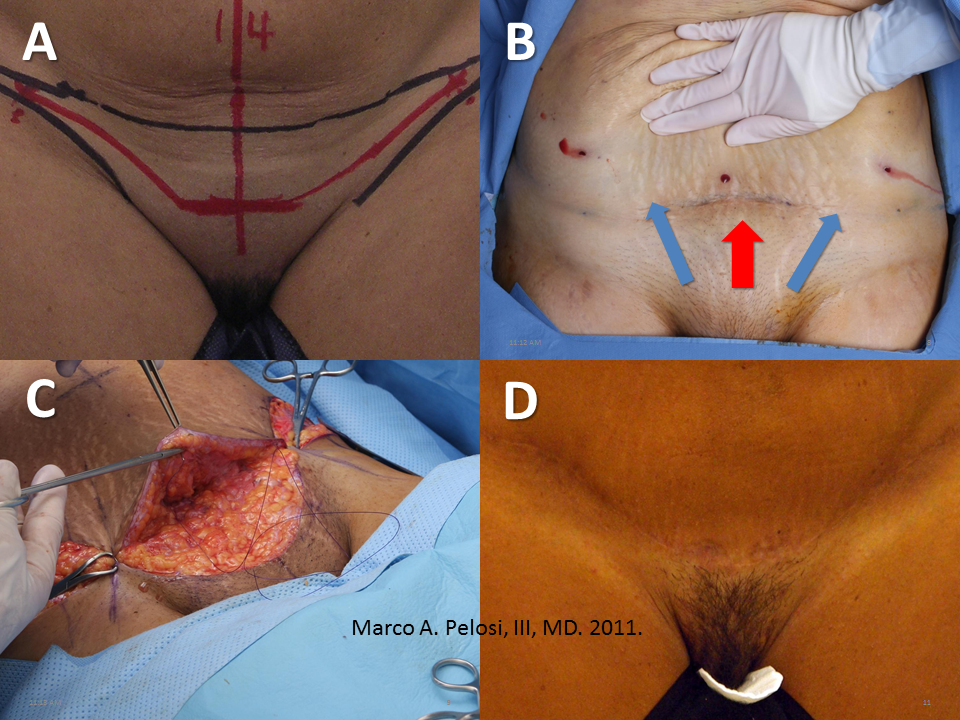
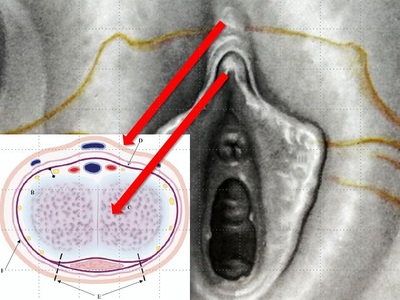
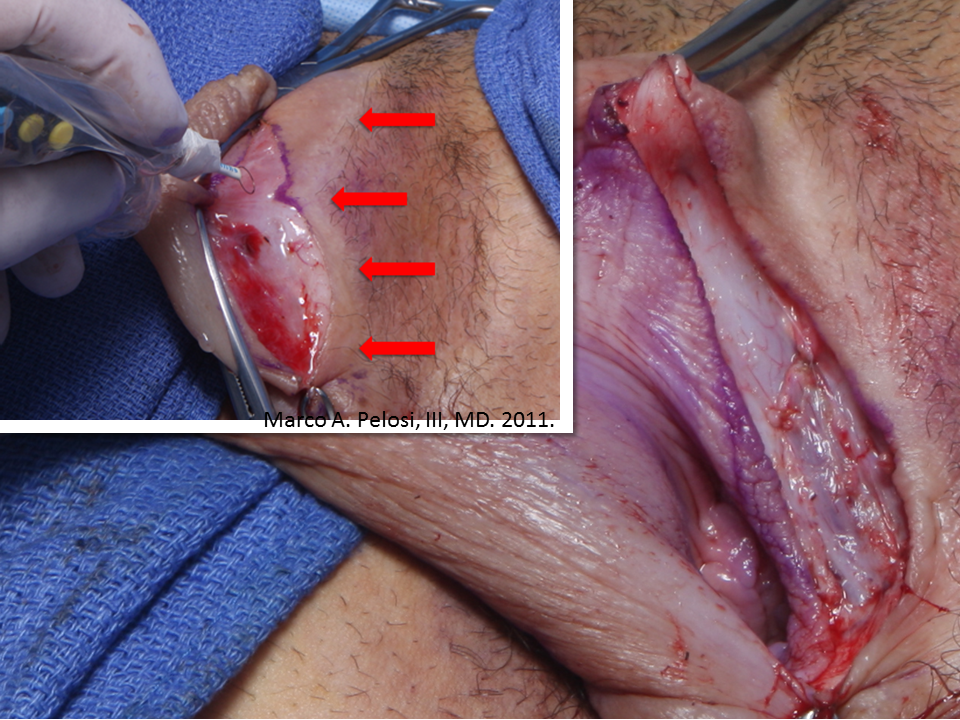
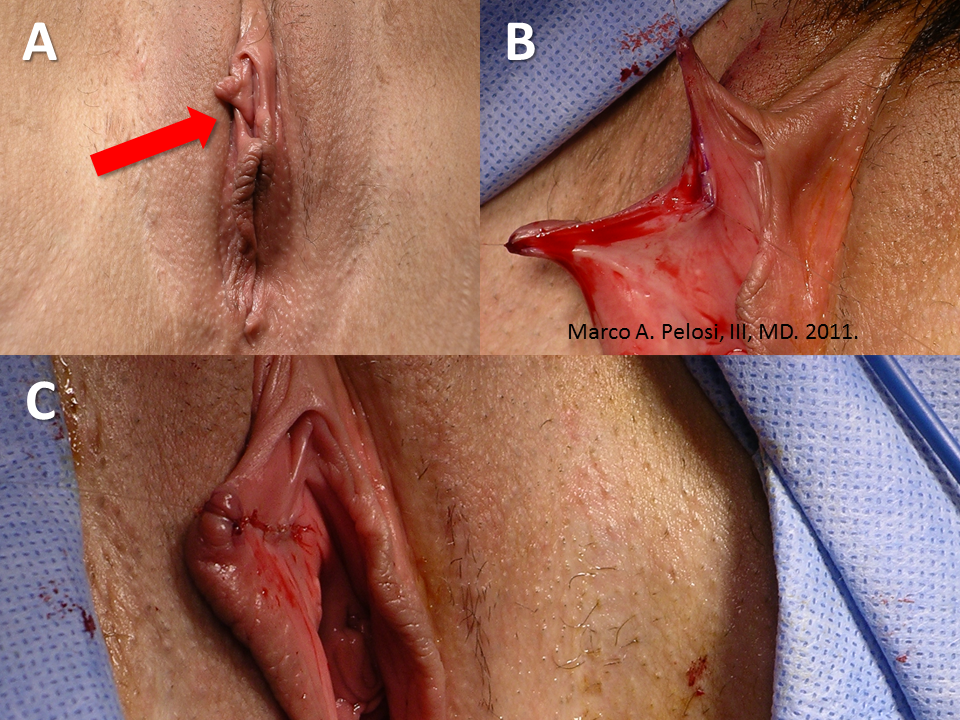
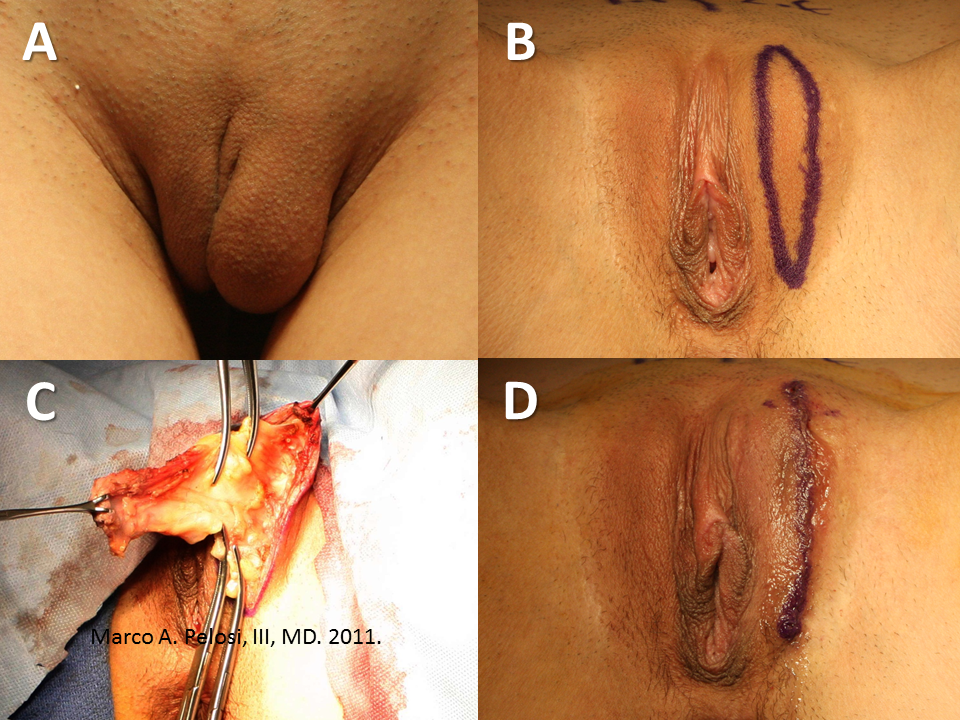
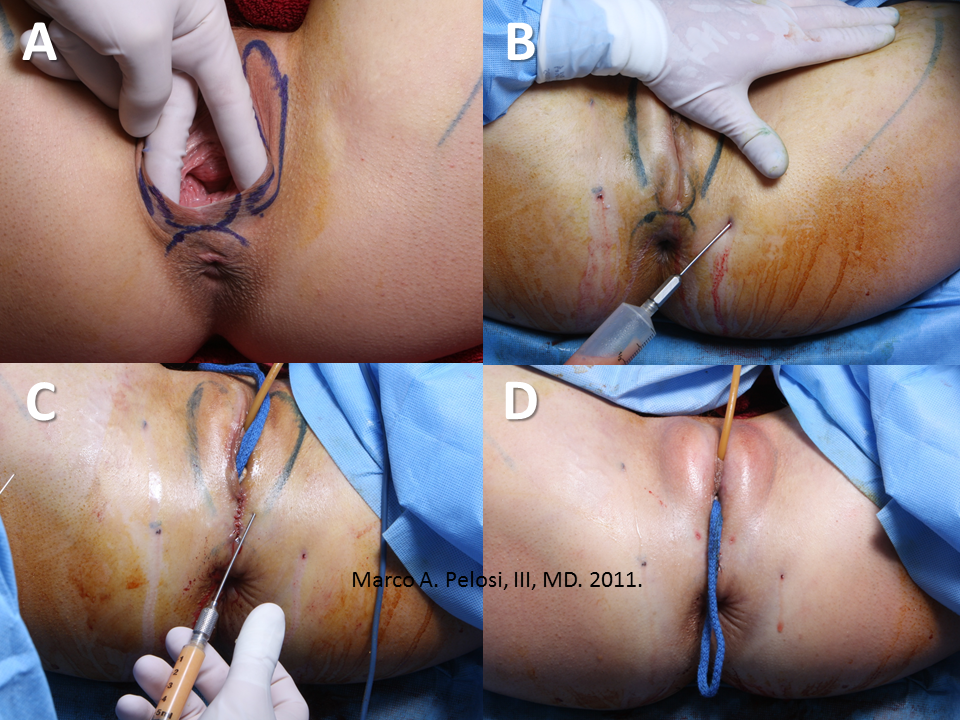
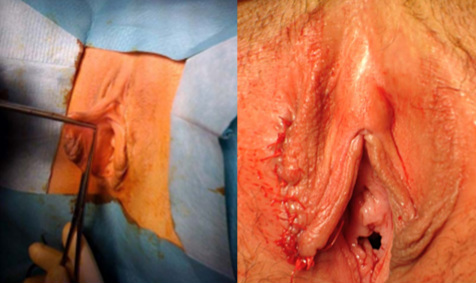
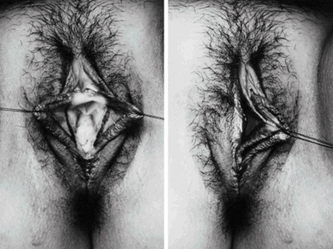
I wrote a review article on cosmetic vaginal surgery for the short-lived internet journal US Obstetrics & Gynecology a while back. With their website gone, the links to this fine manuscript have evaporated into the abyss of The Cloud. Back from the ashes, here it is slightly updated: AbstractA variety of procedures are available for the cosmetic enhancement of the female genitalia. Despite controversy, they continue to grow in popularity. Familiarity with the terminology and spectrum of the aesthetic options described herein permits a realistic assessment of the ways in which the female patient’s concerns may be addressed. There are important aspects of patient evaluation and counseling unique to cosmetic surgery that must be learned by those contemplating the delivery of these services. IntroductionCosmetic vaginal surgery encompasses aesthetic procedures directed at the appearance of the vulvar structures and tightening procedures directed at the reduction of vaginal caliber. The most commonly treated areas are the external vulvar structures. These include the mons pubis, the labia majora and the labia minora which includes the clitoral prepuce. The perineum and the lower third of the posterior vaginal wall are the areas typically operated in vaginal tightening procedures. The anterior vaginal wall does not play a role in vaginal tightening. Hymenoplasty is performed when requested for cultural reasons. Like cosmetic procedures of the face, the breasts and the body, vaginal procedures focus on the elective alteration of normal structures. They are not treatments for medical conditions and offer no health benefits. Unlike these other established cosmetic procedures, the first public wave of cosmetic vaginal surgery emerged from the work of corporate-style entities which branded their procedures and treated their technical knowledge as private intellectual property. Over the past decade, cosmetic vaginal surgery has reached public awareness on par with other cosmetic procedures and a growing number of gynecologists, cosmetic surgeons and plastic surgeons are offering these services to their patients. The reasons behind the increased demand for this type of surgery has been postulated by many groups, but not established by any type of scientific analysis. Many have used this information vacuum as an opportunity to advance or regurgitate chronic agendas against cosmetic surgery in general. Our impression as surgeons performing this type of surgery as well as a wide range of established cosmetic procedures is that the rapid growth of these procedures is due to three factors. First, is timing. The first half of the past decade witnessed the greatest surge in cosmetic medical and surgical volume in history. Yearly statistics monitoring the cosmetic activities of ENT, dermatology and plastic surgery specialists demonstrated a six-fold increase in total cosmetic procedures between 1997 and 2006 (ASAPS, 2007). Cosmetic vaginal surgery emerged during this era and became a component of the intense media coverage which brought cosmetic surgery onto television shows and other media. Second, is the global cultural shift into social media communications as the internet and advanced mobile devices created a level of awareness and information access unprecedented in human history. It is not only possible, but simple, for anyone anywhere to access media on any topic at any time without censorship. Access to services is relatively unimpeded. Third, depilation of the mons pubis has become as popular as that of the legs and axillae in the United States. Once depilated, these areas have now become targets of decoration with tattoos, piercings and surgical modification. A background in gynecology is ideal for evaluating the prospective cosmetic vaginal surgery patient because gynecologic disease or dysfunction may be aggravated if a procedure is performed at the wrong time (e.g. vaginal tightening in a woman who plans on delivering vaginally in the near future or in a woman who has significant pelvic floor defects). However, the evaluation of the cosmetic patient also warrants attention to psycho-social factors which might lead to unrealistic or unachievable expectations such as the presence of body dysmorphic disorder, immaturity, a perfectionist mentality, a cosmetic surgery addiction, a belief that surgery will cure interpersonal problems or a desire to have surgery for the benefit of a partner. These issues are common screening criteria for all cosmetic surgical procedures, but gynecologists who enter this field with a broad knowledge of gynecology, but little familiarity with the cosmetic patient may find these issues to be a new dimension previously unexplored. The Cosmetic Gynecologic AssessmentUnlike the medical patient who seeks relief from disease, deformity or dysfunction, the cosmetic patient must meet be completely healthy in order to be an appropriate candidate for a procedure which offers no health benefit. The well-chosen patient fall into either category ASA I or ASA II of the American Society of Anesthesiologists Physical Status Classification System, but those with specific diseases with a known predisposition to poor healing or increased surgical morbidity such as diabetes or hypertension are best avoided. Hospitalization costs associated with cosmetic procedures, planned or unplanned, are not covered by conventional healthcare insurance. Following the initial conversation regarding the cosmetic request and the requisite psycho-social analysis, the physical examination is conducted. For cosmetic requests involving the vulvar structures or mons pubis, the physical examination is best conducted with the patient standing before a full-length mirror because this is typically the position in which they wish the appearance to be altered. The standard gynecologic dorsal lithotomy position is then assumed to better examine the full extent of the vulvar structures and to conduct a full gynecologic examination include an assessment of any infection which may interfere with the surgical procedure. For vaginal tightening operations there is no need for the standing examination unless there is suspicion of pelvic organ prolapse. However, there is a need to assess the existing width of the levator hiatus and the quality of the puborectalis muscle tone since this will be the focus of these procedures. A common practice is to measure the hiatus in fingerbreadths with the muscles at rest and with the muscles contracted then convert this data to centimeters. Peri-Operative CareAnesthesia requirements for cosmetic vaginal surgery are no different than those for any other vaginal procedure and can be either general, epidural, spinal or intravenous sedation with local block. Prophylactic antibiotics are routinely employed immediately before surgery. Patients are positioned in dorsal lithotomy with the legs supported in boot-type stirrups with mild flexion of the knee. Intermittent pneumatic compression stockings are routinely employed. Indwelling bladder catheterization is employed during most operations. Bladder catheterization is maintained postoperatively for 24 hours in cases where periurethral swelling is anticipated and in cases in which vaginal packing is placed. The Mons PubisThree common cosmetic treatments are available for the mons pubis. The first of these is simple depilation of the pubic hair. The techniques and technologies are the same as those used elsewhere on the body and include laser or intense pulsed light (IPL) treatments administered in a series of sessions over an interval of several months. Multiple sessions are necessary because hair follicles are sensitive to therapy at only certain points in their growth cycle and at any given time, only about 25% of these follicles are in the requisite phase. Modern depilation technologies do not result in total depilation, but greatly reduce the density of hair follicles and the frequency with which any additional depilation maneuvers (shaving, waxing) are needed. The technologies are limited by the degree of melanin and skin pigmentation present and are not advisable for the darkest skin types. Liposuction of the mons pubis is a common procedure for the treatment of excess adiposity and is usually performed in conjuction with abdominal liposuction. The treatment tapers off into the anterior margin of the labia majora. Tumescent local anesthesia – a solution of saline, lidocaine, epinephrine and sodium bicarbonate – is the most common type of anesthetic used for this procedure. Mild postoperative swelling and slight temporary bruising extending to the labia majora are common in the first week after surgery. Mons pubis liposuction is also performed as an adjunct to abdominoplasty when the inferior edge of the incision line is significantly thicker than superior flap. The mons pubis lift is a derivative of abdominoplasty techniques and targets significant laxity in the mons pubis region and sagging of the labia majora as viewed in the standing position. The procedure entails careful controlling of the central tension vectors when planning the resection pattern at the time of abdominoplasty. Whether the procedure is isolated or part of a larger abdominoplasty, excess tension at the lateral angles of the pubic triangle and curving the center of the scar cephalad are two aspects of the surgery which need to be avoided to generate an optimal cosmetic result. These goals are best accomplished with a high lateral tension-style excision pattern. The pubic lift integrates well with mons pubis liposuction. Mons pubis lift with abdominoplasty. A. Surgical markings demonstrate incision line (red) and bikini lines (black). B. Traction is applied to mons pubis after preliminary liposuction has been completed and vectors are studied for adequacy. C. Vectors are reassessed at time of flap closure. D. Appearance at six months post-surgery. The Clitoral RegionLoose, redundant folds of skin lateral to the clitoris are the target of cosmetic excision in this region. This tissue is contiguous with the skin of the clitoral hood (prepuce), but does not function to protect the glans clitoridis. These skin folds may be as large as the main clitoral body and precise dissection in a direction and depth that avoids the path of the clitoral sensory nerves is essential to maintain full sensation. Maintenance of symmetry is another essential aspect of the surgery as the resection of too much skin may pull the clitoral alignment away from the midline. Since this is cosmetic surgery, camouflage of the suture lines is desirable. To this end, incisions across the dorsum of the prepuce along the clitoral shaft should be avoided because they will be visible when the patient is viewed in the standing position. Maintaining incision lines parallel to or within the natural skin folds produces an effective camouflage and is very difficult to detect. When planning surgery of this type in combination with an abdominoplasty or a mons pubis lift, the lift is done first because it frequently produces a tightening of the prepuce in the vertical axis when the mons pubis is placed on cephalad traction. The Labia MinoraReduction labiaplasty of the labia minora is one of the most commonly requested cosmetic vaginal surgery procedures. Common presenting complaints include dissatisfaction with elongated, asymmetric or hyperpigmented labial tissue. Less frequently, patients will request repair of chronic torn labial tissue years subsequent to vaginal delivery. A thorough examination of the labia minora, from a cosmetic perspective, necessitates splaying them laterally onto the labia majora to determine the degrees of hypertrophy, hyperpigmentation and asymmetry which may be present. Proposed excision lines are marked and demonstrated to the patient with a hand mirror. Anteriorly, the planned excision lines may end inferior to, at or beyond the clitoral frenulum. Posteriorly, the excision line may extend toward the fourchette in the midline. When combined reduction labialplasty and vaginal tightening procedures are planned, vaginal tightening is performed first because it involves the resection of the existing fourchette. Laterally, resection should never extend beyond the natural crease between the labium minus and the labium majus because the tension which results may produce gaping of the vaginal introitus and expose the urethra. Suture lines are dressed with topical tissue sealants at the conclusion of surgery and patients are instructed to avoid tight clothing for the first two weeks, to avoid inserting anything in the vagina for six weeks, and to avoid prolonged sitting on the suture lines for six weeks. Local edema and bruising are common in the first two weeks following these operations. Left labia minoraplasty for the relief of sports-related traction pain at the time of a bilateral procedure. Inset illustrates the natural crease between labium minus and labium majus which must be preserved to prevent gaping of the vaginal introitus. Larger photo demonstrates appearance labial base. The left clitoral crus and bulbocavernosus muscle are clearly demonstrated. Right sided reconstructive labia minoraplasty for chronic second-degree tear with associated traction dyspareunia. A. Arrow indicates defect which involves the insertion of the clitoral hood to the labium minus dorsum. B. With the corners of the defect on traction, the scar tissue has been excised in preparation for repair. C. Appearance immediately following a three-layered reconstruction. The Labia MajoraLoose sagging skin, loss of volume, varicosities and unwanted hair are the common complaints of women seeking alteration of labia majora appearance. Redundant skin is best managed by longitudinal ellipsoid resections of skin and subcutaneous fat. Aggressive dissection along the course of the sensory nerve supply to the labia and clitoris should be avoided. Absolute hemostasis is critical in this highly vascular and very elastic tissue as large hematomas can easily develop. Volume loss is addressed by autologous fat transfer into the subcutaneous fat layer. Fat is harvested from any convenient site using conventional liposuction techniques and typically requires less than 50cc for a bilateral augmentation. Fat injections are performed with specialized blunt-tipped needles to avoid the risk of cannulating blood vessels inadvertently. As the fat is injected into the area, it is molded into the desired shape by pressure and massage. Some loss of the implanted fat volume is expected and the need for multiple fat transfer sessions is anticipated. Varicose veins of the vulvar region respond to sclerotherapy in much the same manner as those of the lower extremity. Not infrequently, these varicosities are a source of pelvic pain and a gynecologic workup for pain should rule out other etiologies prior to treatment. Common sclerosing agents such as sodium tetradecyl sulfate are used and administered via small-guage needles attached to tuberculin syringes. The veins are targeted in the standing position and injected in the supine position. The technique is identical to sclerotherapy of the leg varicosities working from proximal to distal veins. A pelvic compression garment is worn for the first week post-injection. Left sided reconstructive labia majoraplasty for a non-communicating hydrocele. A. The extent of the distortion is demonstrated. B. The skin resection margins were marked in the standing position and are demonstrated in dorsal lithotomy. C. Mobilization of the cyst extended along the canal of Nuck and ended at the level of the pubic symphysis. D. Appearance immediately after layered cosmetic reconstruction and Dermabond dressing. Patient presented for augmentation labia majoraplasty with fat injections and treatment of isolated vaginal laxity. A. Attenuation of the perineal body is demonstrated and marked for resection. B. Fat was harvested from the inner thighs using syringe liposuction. C. Following the completion of a modified posterior colpoperineorrhapy, approximately 20 cc of purified fat was injected into each labium majus using a blunt-tipped fat transfer cannula inserted through a needle track incision. D. Immediate post-surgical appearance. Vaginal Tightening (Vaginal Rejuvenation)Procedures for tightening the vaginal caliber are derivations and variations of posterior colporrhaphies and perineorrhaphies. Unlike therapeutic operations targeting significant rectoceles, the focus of these operations is less on the repair of the endopelvic fascia than it is on achieving a reduction of the levator hiatus. The fascial repairs remain important ot the durability of the results, but they are not the technical endpoint for the surgeon. In the absence of advanced degrees of pelvic organ prolapse, mild to moderate degrees of vaginal laxity can be corrected quite adequately by targeting the lower third of the posterior vaginal wall and the perineal body for plication. We do not recommend anterior colporrhaphies for vaginal tightening because they do not add significant tightening at the sites most commonly noted by patients to be loose. Also, gauging the degree of tightening can be tricky in inexperienced hands and those considering offering these surgeries to their patients are well advised to seek specific training in these operations from experts. ConclusionA variety of procedures are available for the cosmetic enhancement of the female genitalia. Despite controversy, they continue to grow in popularity. Familiarity with the terminology and spectrum of the aesthetic options described herein permits a realistic assessment of the ways in which the female patient’s concerns may be addressed. There are important aspects of patient evaluation and counseling unique to cosmetic surgery that must be learned by those contemplating the delivery of these services. References1. Pelosi MA III, Pelosi MA II. Breast augmentation. Obstet Gynecol Clin N Am 2010;37:533-46.
2. Pelosi MA III, Pelosi MA II. Liposuction. Obstet Gynecol Clin N Am 2010;37:507-19. 3. Matlock DL. Letter: Cosmetic therapies in obstetrics and gynecology: putting a toe in the water. Obstet Gynecol 2008;112:703. 4. Pardo J, Sola VD, Ricci PA, Guiloff EF, Freundlich OK. Colpoperineoplasty in women with a sensation of a wide vagina. Acta Obstet Gynecol Scand 2006;85:1125-7. 5. Miklos JR, Moore RD. Labiaplasty of the labia minora: patient indications for pursuing surgery. J Sex Med 2008;5:1492-5. 6. Laube DE. In reply to: Indman PD. Letter to the editor: Cosmetic therapies in obstetrics and gynecology practice: putting a toe in water. Obstet Gynecol 2008; 112: 704-5. 7. DeSousa A. Concerns about cosmetic surgery. Ind J Med Ethics 2007 Vol. 4, No. 4: 171-3. 8. Cosmetic Surgery National Data Bank. 2007 Statistics. New York (NY): American Society for Aesthetic Plastic Surgery; 2009.
1 Comment
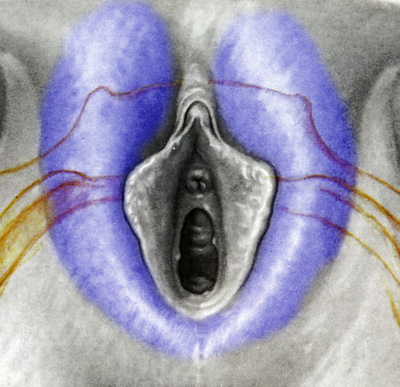
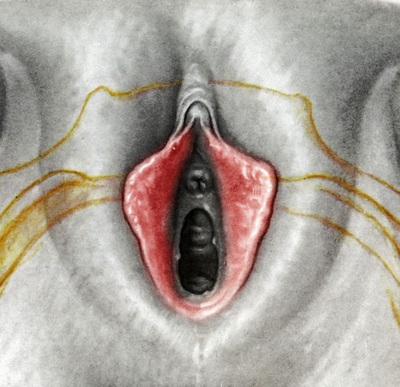
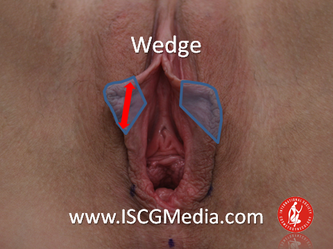
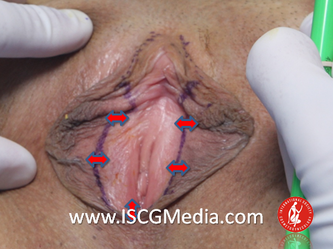
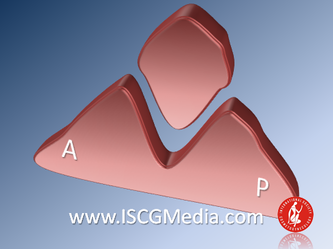
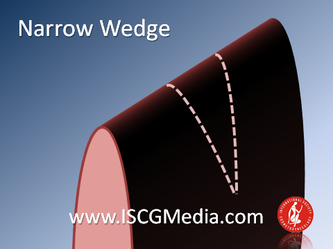
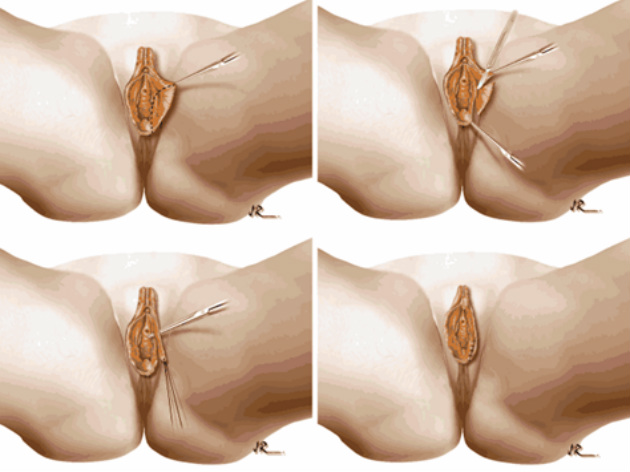
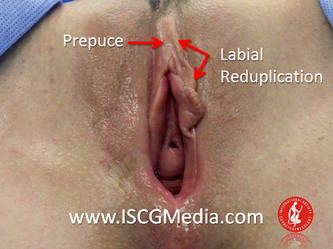
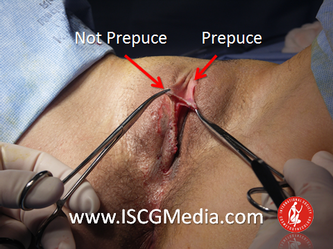
I wanted to share a small sample from an upcoming chapter entitled Cosmetogynecology Note: I took a few liberties with the official version of my work as it will appear in the published version to provide you, the blog reader, with some behind-the-scenes perspectives and anecdotal observations that I usually omit for both brevity and lack of published references from more "learned" discussions. Also, I have included images that exceed those of the to-be-published work because there are no restrictions on quantity here. Bon apetit!  Dr Shirith Sheth Dr Shirith Sheth Shirith S. Sheth, FRCOG Ad Eundem, FACOG (Hon), is an exquisitely skilled, renowned and celebrated gynecologic surgeon from Mumbai, India. He is also a good friend to my surgical team and an individual whom we see much too infrequently. Over a decade ago, we contributed chapters to his excellent book entitled Vaginal Hysterectomy which he co-edited with Dr. John Studd. Several months ago, Dr. Sheth decided that his masterpiece was due for an overhaul and asked if we would be so kind as to update our chapters. He also asked if there was "anything new" that might add to the appeal of the book. Ergo, a chapter on cosmetic gynecology, to be released early next year. We hope you'll like it. LABIA MINORAThe labia minora display a wide range of shapes, sizes, pigmentation and frequent asymmetry. Controlled precise resections are employed to reshape the labia and the skin around the clitoral hood. Some requests are purely cosmetic, others address pain or irritation associated with certain activities such as sex, horseback riding and other sports. Symmetry, balance and comfort are the most common reasons why women request cosmetic alterations of the labia minora. In some instances, treatment is unilateral. Two of these cases presented with complaints of traction pain with various activities. The other two simply disliked the appearance. Can you match the symptoms with the images? - of course not! Myriad techniques for labia minoraplasty abound. They can be categorized into three general groups: (1) linear excisions parallel to the labial edge, (2) wedge excisions perpendicular to the labial edge, and (3) partial-thickness excisions. All of these approaches have been described with variations on the shape and extent of the basic concepts. Linear Labia MinoraplastyModern linear excisions are radically evolved from the simple amputations of antiquity which were originally preferred for their speed in the pre-anesthetic era. The refined cosmetic approach involves a layer-by-layer contoured dissection with hemostatic adjuncts such as vasoconstrictor injections and frequently electrosurgical, radiofrequency or laser coagulation. Linear excisions offer the ability to remove and reshape the entire length and profile of the labial edge. They also allow for precise tension adjustments and typically yield a low-tension suture line and do not generate posterior traction on the clitoral frenulum. If there is a marked color discrepancy between lateral and medial labial skin, this style of labiaplasty may leave an unnatural color transition line along the new labial edge if an aggressive excision is performed. In a full-length excision, 3 to 4 small arterioles will be encountered and require surgical control. Wedge Labia MinoraplastyMarc Laufer (pictured), and William Galvin, pediatric gynecologists at Children's Hospital/ Brigham & Women's Hospital, Boston, Massachussetts, published a 2-case report introducing the wedge labiaplasty technique in 1995 (Adolescent and Pediatric Gynecology 1995;8:39-41). Three years later, Gary Alter, a plastic surgeon from Los Angeles, published a 4-case series introducing the wedge labiaplasty technique. (Annals of Plastic Surgery 1998;40:287-90). In fairness to Alter, I was unable to find Laufer's paper in any medical database using 2013 search technology with a copy of Laufer's paper right in front of me. So how did I find Laufer's obscure paper? He self-referenced it in a 2011 article on pediatric labiaplasty. Wedge excisions offer the ability to preserve the natural labial edge, but cannot reshape the full length of the labial margin. The approach was originally conceived in an effort to reduce scarring and discomfort associated with improperly performed linear excisions (Laufer 1995; Alter 1998). They are a reasonable option when the tissue targeted for excision is limited to a narrow segment of the labium. In a typical wedge excision, a single arteriole is encountered. Wedge excisions near the clitoris have a tendency to draw the frenulum and clitoral hood posteriorly. Attempts to extend the aesthetic reach of this style of labiaplasty by either wider wedging or creative flapping are met by an unacceptably high rate of either incisional dehiscence or tissue necrosis. Partial-Thickness Labia MinoraplastyPartial-thickness skin-only excisions of the labia minora have been proposed with the goal of preserving the labial edge. Two techniques have been described. One of these entails triangular epithelium-only excisions parallel to the long axis of the labium on the medial and again on the lateral aspects. The stroma and vascular supply are not disturbed (Choi et als.). A second approach consists of the resection of a skin-only wedge from the central portion of the labium and consistently leaves a thickened appearance. Clitoral HoodEssentially a component of the labia minora aesthetic unit, the clitoral hood (prepuce) varies greatly in anatomy. Frequently, one finds reduplication of the labia minora extending laterally or bilaterally parallel to the shaft of the clitoris. In other instances, the clitoral hood itself displays loose, redundant folds. Targeted, superficial direct excision of this redundant tissue is individualized. The best cosmetic results are achieved by maintaining suture lines parallel to the clitoral shaft. A cosmetic error, frequently seen with improperly designed linear excisions, is the abrupt termination of the labiaplasty scar at the clitoral hood, leaving a loose redundant mass of periclitoral skin. These require revisionary surgery to essentially complete the procedure. That's it!
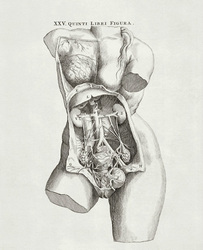
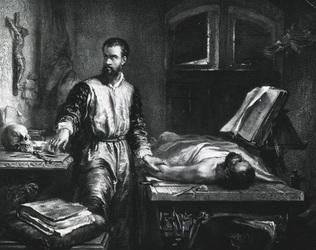
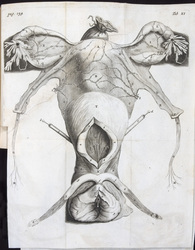
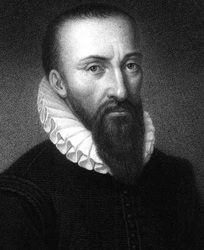
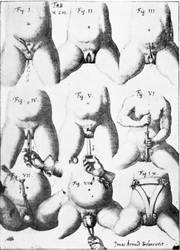
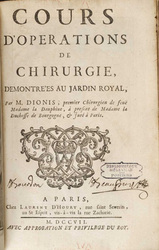
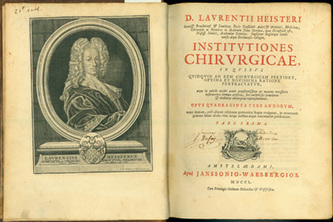
If you want more, you'll have to buy the book or see me in person. Vaginal rejuvenation, or tightening, is over one thousand years old, and it was conceived by women. As mentioned in Part I, the work of the female physician Trotula de Ruggiero of Salerno was published in 1050 AD under the title Treatments for Women. In this volume are five nonsurgical recipes for "restoring" virginity. The section opens as follows: A constrictive for the vagina, so that women may be found to be as though they were virgins, is made in this manner Renowned Medieval historian Monica Green who spent decades researching all extant versions of the Trotula ensemble and Salernan culture prior to her definitive translation opines: It may be that some of these constrictives were meant only to tighten the vagina to the enhance the friction of vaginal intercourse, not necessarily to produce a fake bloodflow of "defloration"; in other words, they may have been intended as aids to sexual pleasure within marriage. The Renaissance brought major advances in anatomic knowledge through cadaveric dissections best represented by Vesalius (1514-1564) at the University of Padua in De Humana Corporis Fabrica. Owing to the invention of the printing press, this knowledge became widely disseminated. However, little if any change in took place in gynecologic surgical technique or instrumentation from that of the Greco-Roman era . Nonetheless, celebrated French surgeon Ambroise Paré (1510-1590) in Gynaeciorium Physicus et Chirurgicus, then his pupil Jacques Guillemeau (1550-1612) in his 1609 text De la Grossesse et Accouchement des Femmes, were first to describe repairs of rectovaginal lacerations at childbirth. Spaniard Roderico a Castro (1546-1627) described clitoridectomy by a horse hair ligature tightened daily in Philosophiae Ac Medicinae Doctoris per Europum notissimi first published in 1604. The first illustration of excision for clitoral hypertrophy was provided by the German surgeon Johann Schultes (aka Scultetus 1595-1645) in Armamentarium Chirurgicum published posthumously in 1655. Pierre Dionis, a Parisian surgeon, described excision of the nymphae (labiaplasty) in his Cours d’opérations de chirurgie (1707) based on his work in the late 1600s in the court of Louis XIV. German military surgeon Lorenz Heister (1683-1758) described labia minoraplasty in full detail in his text, Institutiones Chirurgicae (1739), one of the most popular illustrated surgical texts of the eighteenth century: The nymphae in women are sometimes so large, as not only to hang without the labia pudenda, but also to prove troublesome to them in walking, sitting, and in their conjugal embraces; and may therefore require the surgeon’s assistance. The operator is therefore in the first place to lay the patient in a proper posture, and taking hold of the nymphae with his left hand, he is then to cut off so much of them with a pair of scissors in his right, as he shall judge necessary, taking care to have in readiness styptics for the haemorrhage, and medicines to prevent the patient from fainting. When the operation is over, the wound may be dressed with some vulnerary balsam, and healed without much difficulty in the common method. Key Points1. Vaginal rejuvenation, or tightening, is over one thousand years old, and it was conceived by women.
2. Clitoroplasty, in the Western world, was performed for appearance only through the eighteenth century. 3. Labiaplasty was an established treatment for both symptomatic and aesthetic concerns by the late seventeenth century. |
AuthorMarco A. Pelosi, III, MD, is a cosmetic gynecologist, surgeon, lecturer & cofounder of the ISCG. You may contact him directly at [email protected] Archives
April 2020
Categories
All
|
We are ISCG |
Get to Know Us |
Stay Connected |


































 RSS Feed
RSS Feed
