|
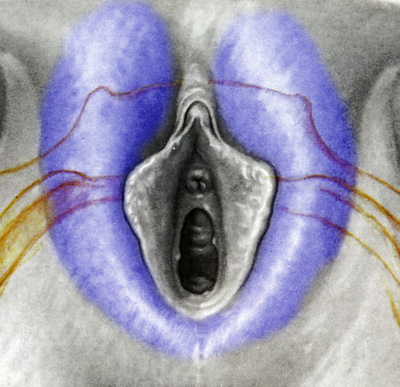
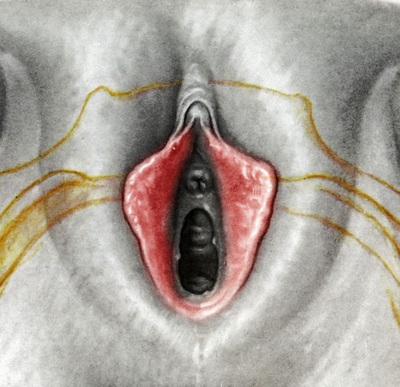
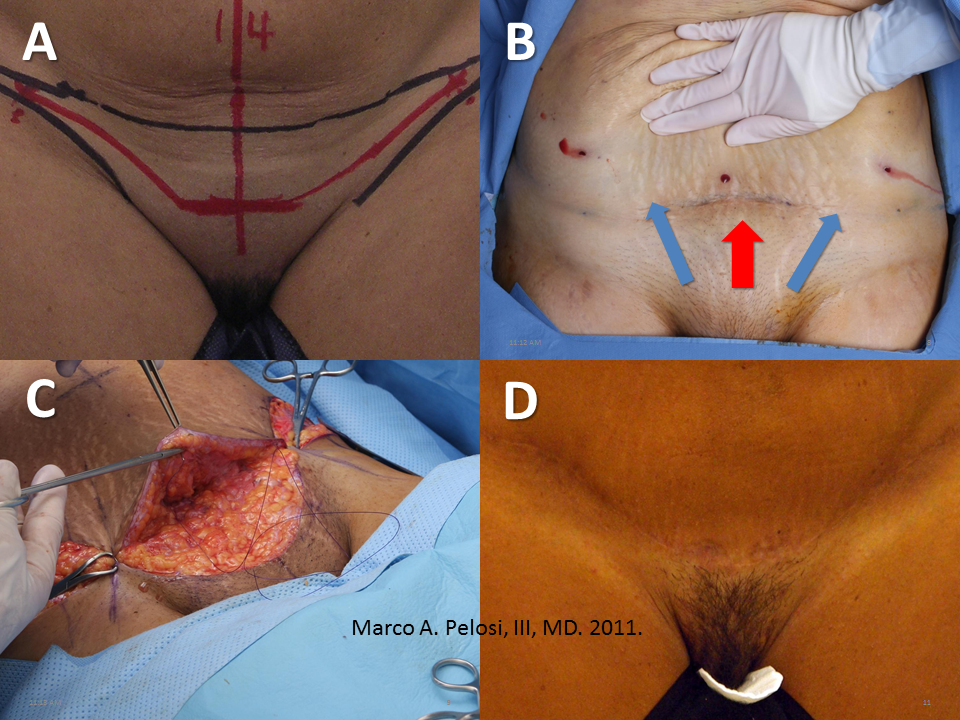
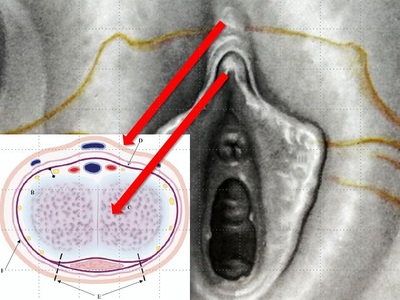
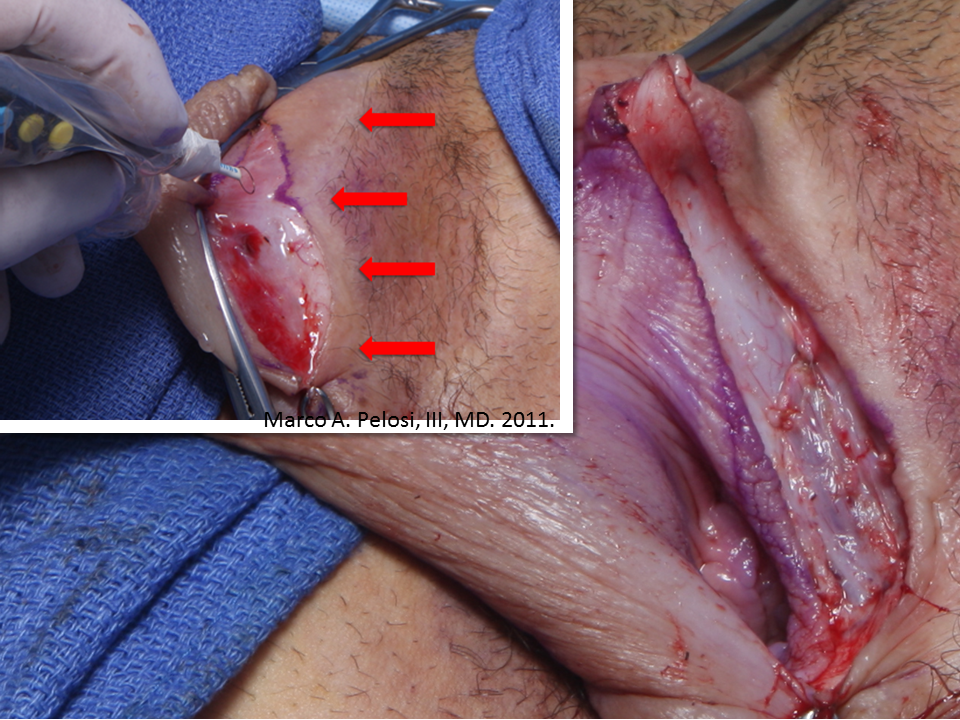
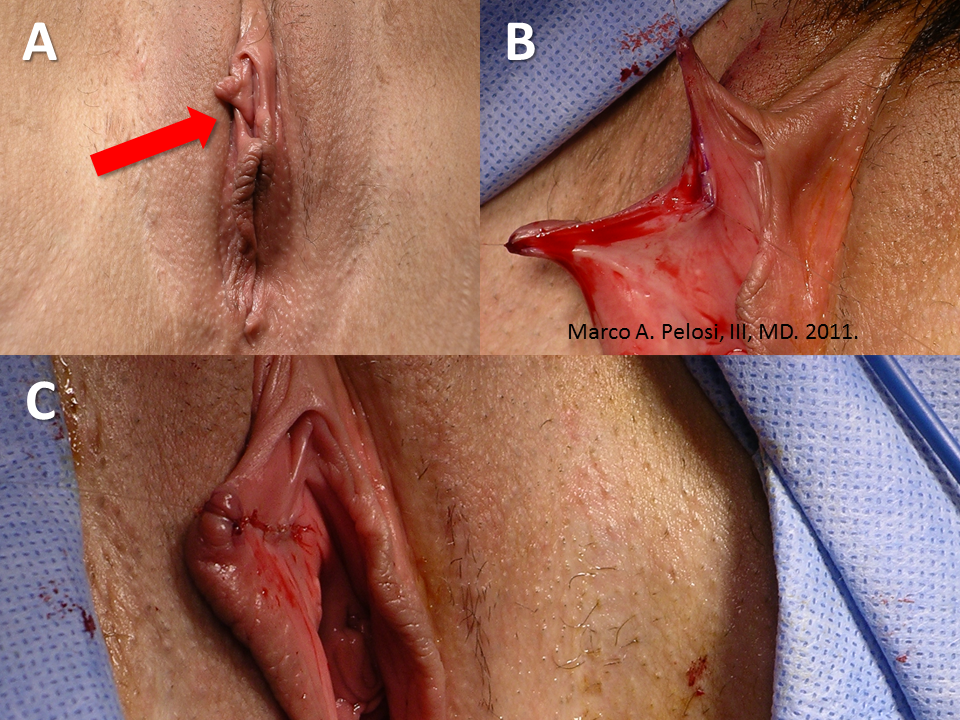
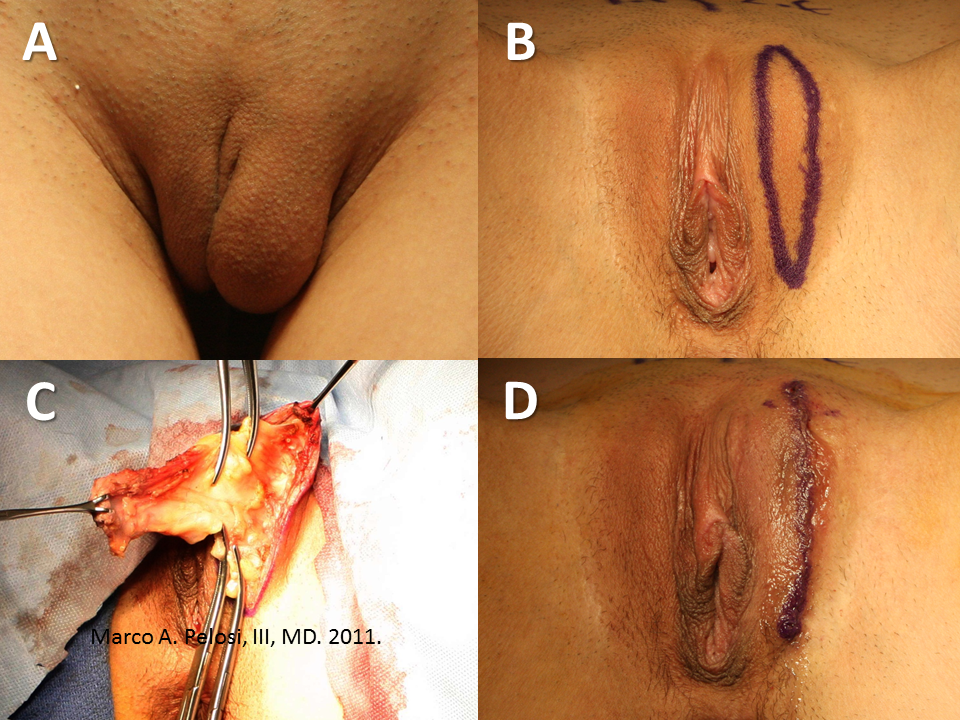
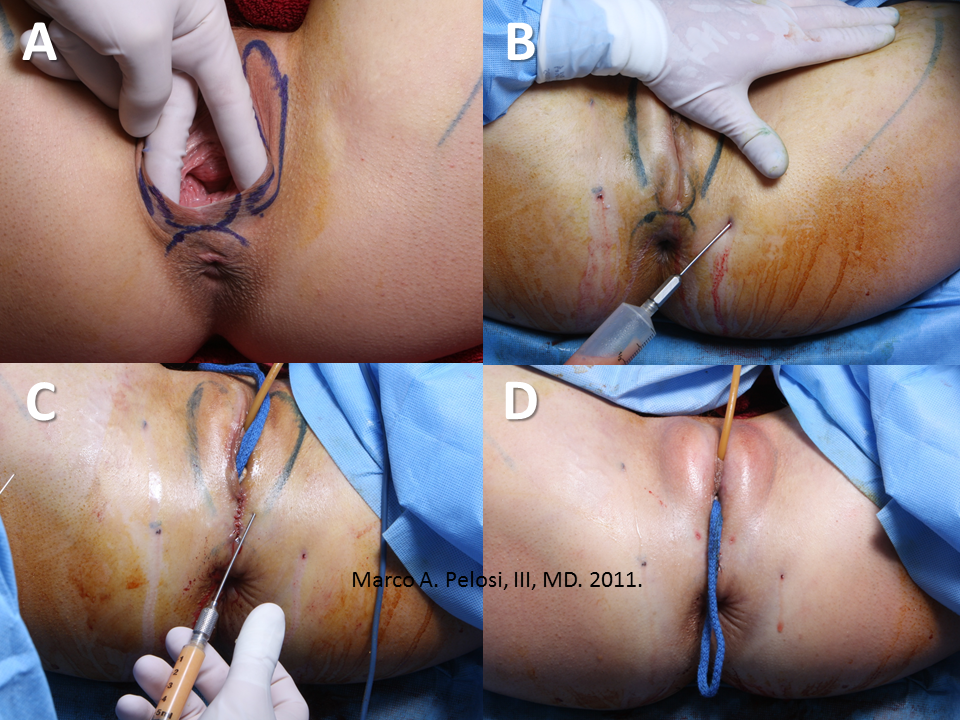
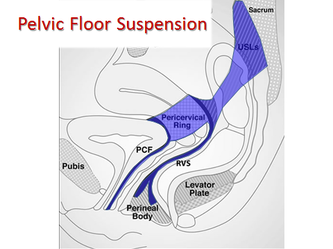
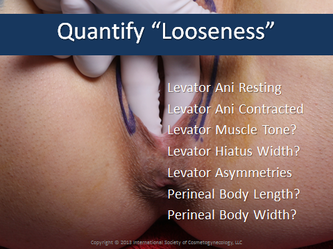
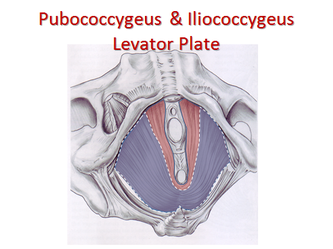
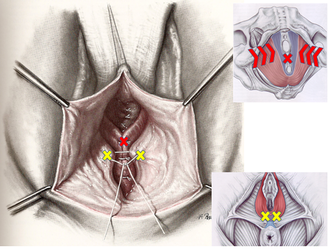
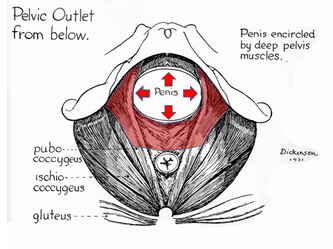
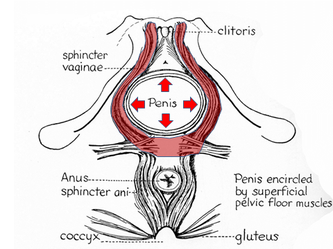
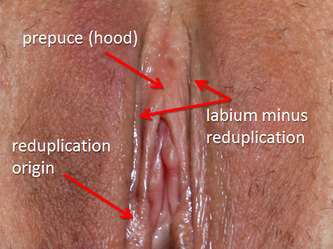
I wrote a review article on cosmetic vaginal surgery for the short-lived internet journal US Obstetrics & Gynecology a while back. With their website gone, the links to this fine manuscript have evaporated into the abyss of The Cloud. Back from the ashes, here it is slightly updated: AbstractA variety of procedures are available for the cosmetic enhancement of the female genitalia. Despite controversy, they continue to grow in popularity. Familiarity with the terminology and spectrum of the aesthetic options described herein permits a realistic assessment of the ways in which the female patient’s concerns may be addressed. There are important aspects of patient evaluation and counseling unique to cosmetic surgery that must be learned by those contemplating the delivery of these services. IntroductionCosmetic vaginal surgery encompasses aesthetic procedures directed at the appearance of the vulvar structures and tightening procedures directed at the reduction of vaginal caliber. The most commonly treated areas are the external vulvar structures. These include the mons pubis, the labia majora and the labia minora which includes the clitoral prepuce. The perineum and the lower third of the posterior vaginal wall are the areas typically operated in vaginal tightening procedures. The anterior vaginal wall does not play a role in vaginal tightening. Hymenoplasty is performed when requested for cultural reasons. Like cosmetic procedures of the face, the breasts and the body, vaginal procedures focus on the elective alteration of normal structures. They are not treatments for medical conditions and offer no health benefits. Unlike these other established cosmetic procedures, the first public wave of cosmetic vaginal surgery emerged from the work of corporate-style entities which branded their procedures and treated their technical knowledge as private intellectual property. Over the past decade, cosmetic vaginal surgery has reached public awareness on par with other cosmetic procedures and a growing number of gynecologists, cosmetic surgeons and plastic surgeons are offering these services to their patients. The reasons behind the increased demand for this type of surgery has been postulated by many groups, but not established by any type of scientific analysis. Many have used this information vacuum as an opportunity to advance or regurgitate chronic agendas against cosmetic surgery in general. Our impression as surgeons performing this type of surgery as well as a wide range of established cosmetic procedures is that the rapid growth of these procedures is due to three factors. First, is timing. The first half of the past decade witnessed the greatest surge in cosmetic medical and surgical volume in history. Yearly statistics monitoring the cosmetic activities of ENT, dermatology and plastic surgery specialists demonstrated a six-fold increase in total cosmetic procedures between 1997 and 2006 (ASAPS, 2007). Cosmetic vaginal surgery emerged during this era and became a component of the intense media coverage which brought cosmetic surgery onto television shows and other media. Second, is the global cultural shift into social media communications as the internet and advanced mobile devices created a level of awareness and information access unprecedented in human history. It is not only possible, but simple, for anyone anywhere to access media on any topic at any time without censorship. Access to services is relatively unimpeded. Third, depilation of the mons pubis has become as popular as that of the legs and axillae in the United States. Once depilated, these areas have now become targets of decoration with tattoos, piercings and surgical modification. A background in gynecology is ideal for evaluating the prospective cosmetic vaginal surgery patient because gynecologic disease or dysfunction may be aggravated if a procedure is performed at the wrong time (e.g. vaginal tightening in a woman who plans on delivering vaginally in the near future or in a woman who has significant pelvic floor defects). However, the evaluation of the cosmetic patient also warrants attention to psycho-social factors which might lead to unrealistic or unachievable expectations such as the presence of body dysmorphic disorder, immaturity, a perfectionist mentality, a cosmetic surgery addiction, a belief that surgery will cure interpersonal problems or a desire to have surgery for the benefit of a partner. These issues are common screening criteria for all cosmetic surgical procedures, but gynecologists who enter this field with a broad knowledge of gynecology, but little familiarity with the cosmetic patient may find these issues to be a new dimension previously unexplored. The Cosmetic Gynecologic AssessmentUnlike the medical patient who seeks relief from disease, deformity or dysfunction, the cosmetic patient must meet be completely healthy in order to be an appropriate candidate for a procedure which offers no health benefit. The well-chosen patient fall into either category ASA I or ASA II of the American Society of Anesthesiologists Physical Status Classification System, but those with specific diseases with a known predisposition to poor healing or increased surgical morbidity such as diabetes or hypertension are best avoided. Hospitalization costs associated with cosmetic procedures, planned or unplanned, are not covered by conventional healthcare insurance. Following the initial conversation regarding the cosmetic request and the requisite psycho-social analysis, the physical examination is conducted. For cosmetic requests involving the vulvar structures or mons pubis, the physical examination is best conducted with the patient standing before a full-length mirror because this is typically the position in which they wish the appearance to be altered. The standard gynecologic dorsal lithotomy position is then assumed to better examine the full extent of the vulvar structures and to conduct a full gynecologic examination include an assessment of any infection which may interfere with the surgical procedure. For vaginal tightening operations there is no need for the standing examination unless there is suspicion of pelvic organ prolapse. However, there is a need to assess the existing width of the levator hiatus and the quality of the puborectalis muscle tone since this will be the focus of these procedures. A common practice is to measure the hiatus in fingerbreadths with the muscles at rest and with the muscles contracted then convert this data to centimeters. Peri-Operative CareAnesthesia requirements for cosmetic vaginal surgery are no different than those for any other vaginal procedure and can be either general, epidural, spinal or intravenous sedation with local block. Prophylactic antibiotics are routinely employed immediately before surgery. Patients are positioned in dorsal lithotomy with the legs supported in boot-type stirrups with mild flexion of the knee. Intermittent pneumatic compression stockings are routinely employed. Indwelling bladder catheterization is employed during most operations. Bladder catheterization is maintained postoperatively for 24 hours in cases where periurethral swelling is anticipated and in cases in which vaginal packing is placed. The Mons PubisThree common cosmetic treatments are available for the mons pubis. The first of these is simple depilation of the pubic hair. The techniques and technologies are the same as those used elsewhere on the body and include laser or intense pulsed light (IPL) treatments administered in a series of sessions over an interval of several months. Multiple sessions are necessary because hair follicles are sensitive to therapy at only certain points in their growth cycle and at any given time, only about 25% of these follicles are in the requisite phase. Modern depilation technologies do not result in total depilation, but greatly reduce the density of hair follicles and the frequency with which any additional depilation maneuvers (shaving, waxing) are needed. The technologies are limited by the degree of melanin and skin pigmentation present and are not advisable for the darkest skin types. Liposuction of the mons pubis is a common procedure for the treatment of excess adiposity and is usually performed in conjuction with abdominal liposuction. The treatment tapers off into the anterior margin of the labia majora. Tumescent local anesthesia – a solution of saline, lidocaine, epinephrine and sodium bicarbonate – is the most common type of anesthetic used for this procedure. Mild postoperative swelling and slight temporary bruising extending to the labia majora are common in the first week after surgery. Mons pubis liposuction is also performed as an adjunct to abdominoplasty when the inferior edge of the incision line is significantly thicker than superior flap. The mons pubis lift is a derivative of abdominoplasty techniques and targets significant laxity in the mons pubis region and sagging of the labia majora as viewed in the standing position. The procedure entails careful controlling of the central tension vectors when planning the resection pattern at the time of abdominoplasty. Whether the procedure is isolated or part of a larger abdominoplasty, excess tension at the lateral angles of the pubic triangle and curving the center of the scar cephalad are two aspects of the surgery which need to be avoided to generate an optimal cosmetic result. These goals are best accomplished with a high lateral tension-style excision pattern. The pubic lift integrates well with mons pubis liposuction. Mons pubis lift with abdominoplasty. A. Surgical markings demonstrate incision line (red) and bikini lines (black). B. Traction is applied to mons pubis after preliminary liposuction has been completed and vectors are studied for adequacy. C. Vectors are reassessed at time of flap closure. D. Appearance at six months post-surgery. The Clitoral RegionLoose, redundant folds of skin lateral to the clitoris are the target of cosmetic excision in this region. This tissue is contiguous with the skin of the clitoral hood (prepuce), but does not function to protect the glans clitoridis. These skin folds may be as large as the main clitoral body and precise dissection in a direction and depth that avoids the path of the clitoral sensory nerves is essential to maintain full sensation. Maintenance of symmetry is another essential aspect of the surgery as the resection of too much skin may pull the clitoral alignment away from the midline. Since this is cosmetic surgery, camouflage of the suture lines is desirable. To this end, incisions across the dorsum of the prepuce along the clitoral shaft should be avoided because they will be visible when the patient is viewed in the standing position. Maintaining incision lines parallel to or within the natural skin folds produces an effective camouflage and is very difficult to detect. When planning surgery of this type in combination with an abdominoplasty or a mons pubis lift, the lift is done first because it frequently produces a tightening of the prepuce in the vertical axis when the mons pubis is placed on cephalad traction. The Labia MinoraReduction labiaplasty of the labia minora is one of the most commonly requested cosmetic vaginal surgery procedures. Common presenting complaints include dissatisfaction with elongated, asymmetric or hyperpigmented labial tissue. Less frequently, patients will request repair of chronic torn labial tissue years subsequent to vaginal delivery. A thorough examination of the labia minora, from a cosmetic perspective, necessitates splaying them laterally onto the labia majora to determine the degrees of hypertrophy, hyperpigmentation and asymmetry which may be present. Proposed excision lines are marked and demonstrated to the patient with a hand mirror. Anteriorly, the planned excision lines may end inferior to, at or beyond the clitoral frenulum. Posteriorly, the excision line may extend toward the fourchette in the midline. When combined reduction labialplasty and vaginal tightening procedures are planned, vaginal tightening is performed first because it involves the resection of the existing fourchette. Laterally, resection should never extend beyond the natural crease between the labium minus and the labium majus because the tension which results may produce gaping of the vaginal introitus and expose the urethra. Suture lines are dressed with topical tissue sealants at the conclusion of surgery and patients are instructed to avoid tight clothing for the first two weeks, to avoid inserting anything in the vagina for six weeks, and to avoid prolonged sitting on the suture lines for six weeks. Local edema and bruising are common in the first two weeks following these operations. Left labia minoraplasty for the relief of sports-related traction pain at the time of a bilateral procedure. Inset illustrates the natural crease between labium minus and labium majus which must be preserved to prevent gaping of the vaginal introitus. Larger photo demonstrates appearance labial base. The left clitoral crus and bulbocavernosus muscle are clearly demonstrated. Right sided reconstructive labia minoraplasty for chronic second-degree tear with associated traction dyspareunia. A. Arrow indicates defect which involves the insertion of the clitoral hood to the labium minus dorsum. B. With the corners of the defect on traction, the scar tissue has been excised in preparation for repair. C. Appearance immediately following a three-layered reconstruction. The Labia MajoraLoose sagging skin, loss of volume, varicosities and unwanted hair are the common complaints of women seeking alteration of labia majora appearance. Redundant skin is best managed by longitudinal ellipsoid resections of skin and subcutaneous fat. Aggressive dissection along the course of the sensory nerve supply to the labia and clitoris should be avoided. Absolute hemostasis is critical in this highly vascular and very elastic tissue as large hematomas can easily develop. Volume loss is addressed by autologous fat transfer into the subcutaneous fat layer. Fat is harvested from any convenient site using conventional liposuction techniques and typically requires less than 50cc for a bilateral augmentation. Fat injections are performed with specialized blunt-tipped needles to avoid the risk of cannulating blood vessels inadvertently. As the fat is injected into the area, it is molded into the desired shape by pressure and massage. Some loss of the implanted fat volume is expected and the need for multiple fat transfer sessions is anticipated. Varicose veins of the vulvar region respond to sclerotherapy in much the same manner as those of the lower extremity. Not infrequently, these varicosities are a source of pelvic pain and a gynecologic workup for pain should rule out other etiologies prior to treatment. Common sclerosing agents such as sodium tetradecyl sulfate are used and administered via small-guage needles attached to tuberculin syringes. The veins are targeted in the standing position and injected in the supine position. The technique is identical to sclerotherapy of the leg varicosities working from proximal to distal veins. A pelvic compression garment is worn for the first week post-injection. Left sided reconstructive labia majoraplasty for a non-communicating hydrocele. A. The extent of the distortion is demonstrated. B. The skin resection margins were marked in the standing position and are demonstrated in dorsal lithotomy. C. Mobilization of the cyst extended along the canal of Nuck and ended at the level of the pubic symphysis. D. Appearance immediately after layered cosmetic reconstruction and Dermabond dressing. Patient presented for augmentation labia majoraplasty with fat injections and treatment of isolated vaginal laxity. A. Attenuation of the perineal body is demonstrated and marked for resection. B. Fat was harvested from the inner thighs using syringe liposuction. C. Following the completion of a modified posterior colpoperineorrhapy, approximately 20 cc of purified fat was injected into each labium majus using a blunt-tipped fat transfer cannula inserted through a needle track incision. D. Immediate post-surgical appearance. Vaginal Tightening (Vaginal Rejuvenation)Procedures for tightening the vaginal caliber are derivations and variations of posterior colporrhaphies and perineorrhaphies. Unlike therapeutic operations targeting significant rectoceles, the focus of these operations is less on the repair of the endopelvic fascia than it is on achieving a reduction of the levator hiatus. The fascial repairs remain important ot the durability of the results, but they are not the technical endpoint for the surgeon. In the absence of advanced degrees of pelvic organ prolapse, mild to moderate degrees of vaginal laxity can be corrected quite adequately by targeting the lower third of the posterior vaginal wall and the perineal body for plication. We do not recommend anterior colporrhaphies for vaginal tightening because they do not add significant tightening at the sites most commonly noted by patients to be loose. Also, gauging the degree of tightening can be tricky in inexperienced hands and those considering offering these surgeries to their patients are well advised to seek specific training in these operations from experts. ConclusionA variety of procedures are available for the cosmetic enhancement of the female genitalia. Despite controversy, they continue to grow in popularity. Familiarity with the terminology and spectrum of the aesthetic options described herein permits a realistic assessment of the ways in which the female patient’s concerns may be addressed. There are important aspects of patient evaluation and counseling unique to cosmetic surgery that must be learned by those contemplating the delivery of these services. References1. Pelosi MA III, Pelosi MA II. Breast augmentation. Obstet Gynecol Clin N Am 2010;37:533-46.
2. Pelosi MA III, Pelosi MA II. Liposuction. Obstet Gynecol Clin N Am 2010;37:507-19. 3. Matlock DL. Letter: Cosmetic therapies in obstetrics and gynecology: putting a toe in the water. Obstet Gynecol 2008;112:703. 4. Pardo J, Sola VD, Ricci PA, Guiloff EF, Freundlich OK. Colpoperineoplasty in women with a sensation of a wide vagina. Acta Obstet Gynecol Scand 2006;85:1125-7. 5. Miklos JR, Moore RD. Labiaplasty of the labia minora: patient indications for pursuing surgery. J Sex Med 2008;5:1492-5. 6. Laube DE. In reply to: Indman PD. Letter to the editor: Cosmetic therapies in obstetrics and gynecology practice: putting a toe in water. Obstet Gynecol 2008; 112: 704-5. 7. DeSousa A. Concerns about cosmetic surgery. Ind J Med Ethics 2007 Vol. 4, No. 4: 171-3. 8. Cosmetic Surgery National Data Bank. 2007 Statistics. New York (NY): American Society for Aesthetic Plastic Surgery; 2009.
1 Comment
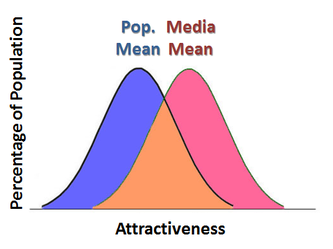
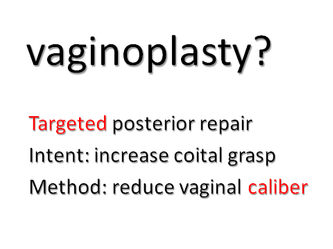
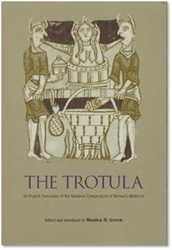
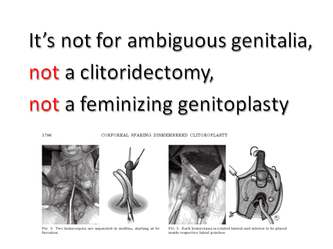
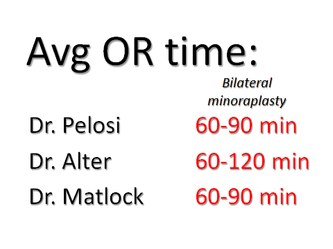
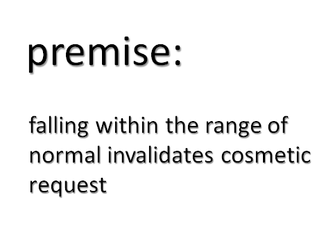
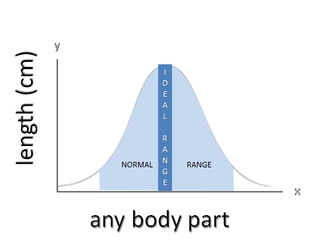
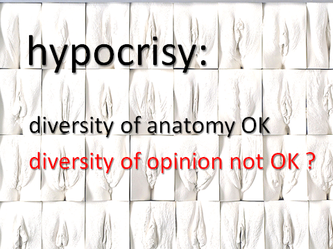
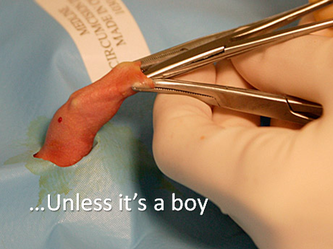
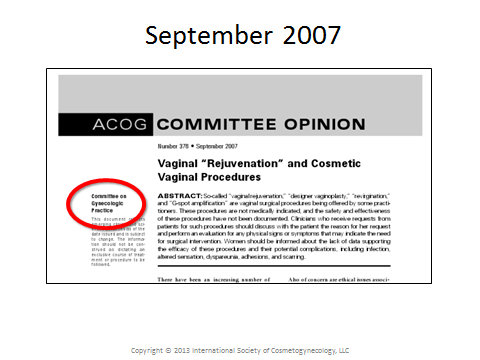
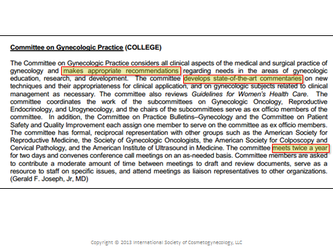
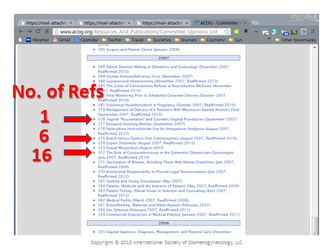
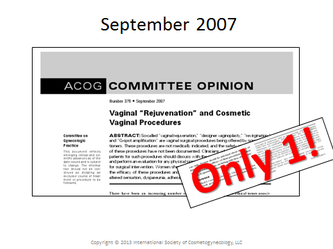
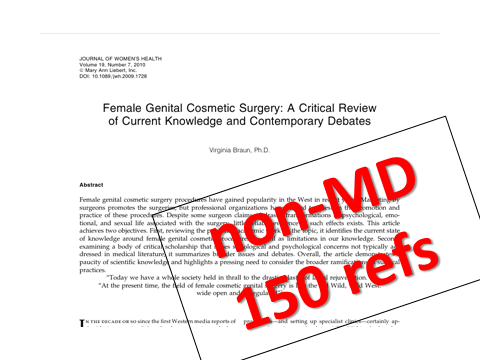
This is the complete presentation delivered at Baystate Medical Center, Springfield, Massachusetts, on March 20, 2013. View the references here. View the slides-only YouTube version here. It is the pro stance in a pro-con debate on cosmetic gynecology delivered to an audience of non-cosmetic medical professionals, mostly gynecologists. Beauty is sometimes described as a cultural currency. Nature distributes beauty randomly & this doesn’t sit well with our sense of wanting to treat individuals equally. But this is simply an observation. The Egyptians were great admirers of beauty and left us with a large historical record of their efforts to enhance appearance. The ancient Greeks and the Romans personified their visions of beauty in the statues of their gods. The Greek root of the word “aesthetics” means that which relates to sensory perception. Aesthetics is the application of values and judgments to that which we sense, it’s totally subjective. Beautiful, good, bad, ugly, are applied to anything we perceive. We do this universally. But why do we do this? It is theorized that our thinking processes adapted along with our bodies to ensure survival in the primitive world of the Stone Age. Our brains evolved to do this. The study of this topic is termed evolutionary psychology. It’s a relatively new field, but it is gaining incredible traction among scholars in many disciplines. We're only going cover a few of the relevant aspects of evolutionary psychology as they relate to cosmetic surgery. Evolution favors processes that maximize the reproductive potential of the population as a whole. Individuals who display reproduction-positive thinking processes will be more likely to reproduce & pass on those thinking processes to future populations. Over many generations and hundreds of thousands of years, the majority of individuals in future populations will display these traits. Aesthetic standards of human beauty are an example of an evolved thinking process. These unwavering qualities of human appearance have been deemed beautiful, attractive and desirable in every culture from the beginning of recorded history. These standards have always existed and they are NOT arbitrary. They are a good complexion, symmetrical features, and youth. But why are these the standards...? Because they’re blatant displays of reproductive mate value. They’re not perfect markers by any means, but if you’re back in the primordial savannah of the Stone Age, attraction to young, symmetrical, & smooth-skinned mates gives you the best reproductive odds. Complexion, symmetry, & youth are the universal standards of beauty. Psychologists, anthropologists, sociobiologists and others have studied people from vastly different cultures. All of them have come the same conclusion. Study after study demonstrates consistency in judging beauty. Photographs are shown to people from different cultures yet they all consistently agree on which people are most beautiful. We don’t learn what beauty is, we know what beauty is…and it’s not in the eye of the beholder... This startling revelation has been documented consistently in psychological studies using photographs of faces judged attractive by adults. One study demonstrated this in 3-to-6 month-olds. Another study, by one of the giants in this field, Judith Langlois, showed it in 2-to-6 month-olds. A study in the late 1990s showed this tendency in newborns less than one week old. One week old babies have standards of beauty. And it’s the nature of both sexes. Male or female, it’s seems unnatural to be attracted to anything else. Let’s discuss the relationship between standards of beauty, which are natural, and the media, which is man-made. Is the media really creating unhealthy stereotypes that otherwise wouldn’t exist? Does the media really decide what beauty is? If we suppose that advertising defines beauty, then we have to presuppose that complexion, symmetry and youth have no intrinsic attraction to begin with. Does anybody really believe that? Newborn infants don’t believe that. Stone Age man didn’t believe that. The ancient Egyptians didn’t believe that. And marketing firms don’t believe that either. So what’s their angle? They hope that your attraction to complexion, symmetry & youth will spill over onto their product if it’s attached to it... Thank Dr. Pavlov and his dogs for the concept. Advertising is all about getting attention. Catering to our natural attractions has always been the solid bet. The problem with the media is perceptual contrast. What that means is that to outcompete each other for attention, competitors need to use increasingly attractive people to succeed. If you overexpose yourself to the media you might develop a distorted sense of what constitutes an average level of attractiveness, but you’re still attracted to complexion, symmetry and youth. Portable technology attached to media distribution networks overexposes us to the media if we overuse it. The Greek origin of the word “cosmetic” means to adorn or to make beautiful. Cosmetic relates to the process of enhancing something to make it more aesthetic. The term aesthetic surgery is a misnomer – what it really implies is that the surgery itself, like a ballet is beautiful to watch regardless of what’s being done. It has no reference to intent. Plastic means simply to reshape. It too, is without reference to the intent of the reshaping effort. If we use language precisely, then cosmetic surgery is the only term that appropriately defines surgery done with the intent to enhance aesthetics. Like advertising, cosmetic medicine, surgery and products promote complexion, symmetry and youth. But they promote it as something that you can participate in. As a global culture, we don’t just accept cosmetic surgery & medicine. We celebrate it and we participate in it…because it aligns with our attraction to complexion, symmetry and youth. Just like the mirror in your purse, like the braces on your teeth, like the paint on your hair. There has never been a shortage of opinion on cosmetic surgery, but in every culture that has ever existed people have willingly availed themselves of the methods and technologies available at that time to pursue enhanced complexion, symmetry and youth. Some people don’t like cosmetic surgery, and they don’t like that other people like cosmetic surgery. And they don’t like that people do cosmetic surgery, but since our culture tolerates cosmetic surgery they try to attach cosmetic surgery to things that people don’t like to try to convince people to think like they do. They claim that cosmetic surgery is equivalent to false advertising. Nobody likes false advertising. Sure, there are plenty of examples of false advertising in cosmetic surgery, in non-cosmetic surgery, and in every industry that advertises, but that’s a judgment on advertising, not on the merits of surgery itself. Some say that cosmetic surgery is porn-driven. It’s not. Porn is media. They want to display complexion, symmetry and youth to sell their product just like any other type of media. It’s another example of advertising promoting universal innate standards. If porn were the global arbiter of style, then we could also make the case that leanness, bleached hair, overdone lips, breast implants and fake orgasms are porn driven too. Don’t try to argue that pornography has ever set standards of beauty. Porn is simply another messenger of the innate message of complexion, symmetry and youth. Some people allege that since their elders didn’t discuss cosmetic surgery, that it’s a new fad. Today’s Baby Boomers went through puberty in the 1950s. The parents of that generation were raised to consider many desires as things to remain unspoken & technology didn’t permit any outlet for information or access to products and services that exist today so that argument doesn’t hold up well at all to scrutiny. Mom’s generation and Stone Age man would have behaved identically to today’s generation if they had access to our knowledge and technology. Let's explore the aesthetics of cosmetic gynecology in the light of what we know about human nature. Despite the obvious fact that the genital area requires effort to make it viewable, and that not everyone chooses it to make it viewable, those who do view it from an aesthetic angle apply the same standards of beauty we are all born with. When they view the genital area through the lens of complexion, symmetry and youth, they will develop an opinion. Whatever that opinion is, they may choose to express that opinion by leaving nature alone, by decorating it, or by altering it with or without the aid of a surgeon. If your opinion becomes your obsession you’ll need the services of a psychiatrist. If not, you might visit someone like me. This thought process applies to any part of the body. Anyone who provides cosmetic services will tell you that the key to a successful outcome is in setting a realistic expectation. Cosmetic expectations are unique to the individual & they can’t be measured like treatment outcomes because they are opinions. You can perform identical cosmetic surgeries on identical twins with perfect healing, but the one who expected something else will not be happy. That being said, public displays of some body parts are more ubiquitous than others so that there is a greater general awareness of the variety that exists in any dimension of a given part that is more widely displayed. Thankfully, displays such as "The Great Wall of Vagina," by artist Jamie McCartney, are permitting previously difficult- to-view areas become more publicly viewable. Clearly, this allows for more robust opinions and therefore better decision making. Most of the anti- cosmetic vaginal surgery noise comes from Great Britain. A small group of critics gets quoted widely. Their real gripe is that their socialized medicine National Health Service is getting stuck with the bill for cosmetic vaginal procedures under the guise of bogus medical indications. Australia and New Zealand have similar socialized healthcare & they mimic the British critics. It’s about limited money better spent elsewhere. I would agree wholeheartedly that the cost of cosmetic surgery should come out of the patient’s pocket, but everything else they claim is poorly argued & unsubstantiated. Cosmetic gynecology is a group of procedures. The efficacy of any procedure is completely dependent on what is expected to happen via the procedure. These procedures share the features of many existing procedures in therapeutic gynecology & the risk profile should be similar provided the surgeon has experience in the relevant therapeutic operations. There is no single component of any cosmetic gynecology procedure that doesn't already exist in therapeutic gynecologic surgery. These are general categories of cosmetic vaginal surgery in my current practice. Cosmetic vaginal surgery is not intended to produce or enhance orgasms. Some say that a gaping vagina isn’t a problem if it lacks pain, bowel dysfunction, or urinary dysfunction. They dismiss the importance of vaginal sensation as something that benefits only the male partner & that women could care less. This might apply to some women, but it doesn’t apply to many, many others. But if you don’t ask them, they won’t tell you. The concept of tightening the vagina to enhance sex is over 1,000 years old. The book, Treatments for Women, part of a popular medieval ensemble of books known as the Trotula was written by a woman in Salerno, Italy in 1050 AD. It lists 5 recipes for tightening the vagina with constrictive agents. Arnold Kegel wrote extensively of vaginal laxity and sex. He didn’t think that vaginal laxity was a bogus, male-oriented concern. Increasing vaginal sensation, or coital grasp, is not the same thing as producing or augmenting an orgasm, but that doesn’t mean that some women don’t enjoy improving their sensation, Especially if it has decreased greatly over time. I had a vaginal delivery, kegels don’t work, I don’t have any of the problems on your pelvic floor checklist & I’m healthy. Is there anything you can do? A woman may have a tight vagina, a gaping vagina, or anything in between, but this is the most common story I hear. I saw a patient in consultation yesterday who was belittled and dismissed by a “pelvic floor surgeon” for raising these concerns & it’s not the first time. Thanks to a general misunderstanding of somebody’s Committee Opinion, many gyns are uncomfortable treating this woman further and even hesitate to inquire about the sex life of their established patients – don’t ask, don’t tell, or go to hell. They’ll either send her my way or tell her nothing can be done. Sad, but true. I hear these stories all the time. In my practice, this patient gets a full pelvic floor evaluation which every gynecologist should know how to do and her kegel technique gets checked for adequacy. That's the starting point. The method of a vaginoplasty is to tighten the caliber of the lower or distal vagina via posterior colporrhaphy and perineorrhaphy. This can only be done effectively if the pelvic floor suspension is relatively intact and the endpoint is defined. This can only be done effectively if the amount of tightening is measured with precision. If not you’ll need to repair the pelvic floor a preliminary step. If you skip the pelvic floor repairs, the existing floor damage might get worse or your tightening procedure might fail. The bottom line: don’t do vaginoplasties if you’re unfamiliar with these types of repairs unless you get someone experienced in these procedures to help you. The procedures don't fail in achieving the goals they are designed to accomplish. Failure is in choosing the wrong procedure for the wrong reasons. Labiaplasty is performed for various reasons, it’s not always bilateral, it’s not always excisional, and the anatomy varies widely. If we’re going to discuss labiaplasty we need to keep these things in mind. Especially since the procedure may involve just a little bit of surgery or something more involved. Also, labiaplasty is not a new operation, and neither is "cosmetic" a new indication. The first labiaplasties were done in seventh century AD for aesthetic reasons as well as for symptomatic ones, but not necessarily for both together. This knowledge has been widely available for over three hundred years. The British opponents of cosmetic vaginal surgery have attempted to extrapolate the complications of extensive surgery performed on newborns in the 1970s by techniques abandoned in the 1980s as potential complications of cosmetic labiaplasty on normally developed adult women. All of these troublesome effects of intersex surgery are related to nerve damage associated with partial amputation of the clitoris, folding of the clitoral shaft, or with the creation of false labia from surrounding tissue. None of this bears any similarity to cosmetic labiaplasty nor to cosmetic alterations of the loose skin around the clitoral hood which do not impinge upon the clitoral nerve supply. I don’t like the way they protrude. They don’t cause any discomfort whatsoever... This is a pure cosmetic request. Her request is not about sexual function. She needs to understand that, you need to understand that. The intent of cosmetic labiaplasty is to achieve the anatomic endpoint requested by the patient. If the request or expectations are unrealistic, the intent will not be realized. They bother me... This is either a pure cosmetic request in disguise or a valid complaint. Evaluation for causes of vulvar pain is the first step. Sadly, if labiaplasty is required many physicians and all insurance companies will deny the request. There is a misconception among gynecologists and other surgeons that labiaplasty is a quick and easy procedure. They believe that the procedure consists of a crude amputation with oversewing of the labial edge. It is true that butchery of that sort can be accomplished quickly. But that is not cosmetic labiaplasty, that is labial amputation & it will never yield satisfactory aesthetic results. Sadly, I've seen the technique used on documentaries painting labialplasty in a negative light. A real cosmetic labiaplasty takes thoughtful aesthetic planning, anatomic caution, and meticulous technique. This takes time, patience and skill. It's not a coincidence that those who perform a large volume of cosmetic labiaplasties take their time. Another poorly constructed argument by the British opponents of cosmetic labiaplasty postulates that since labia vary greatly in dimensions and patients requesting cosmetic labiaplasty fall generally within the normal range of measurements, they shouldn't be permitted to alter these dimensions. Not only is this argument absurd & inconsistent when one considers that the majority of all cosmetic requests on any part of the body involve structures which fall within the normal range of dimensions, but it completely misses the point that those who request cosmetic alterations wish to be in a specific ideal range within the normal range. It's hypocritical & patriarchal when these small groups with extreme ideas intolerantly criticize those who have a differing opinion on cosmetic surgery and they remain silent on parallel procedures performed performed upon males or upon other body parts. The topics of monsplasty (liposuction and/or surgical lifting & tightening) and hymenplasty were listed, but not discussed due to time constraints. Those who are unfamiliar with cosmetic surgery fees claim that prices seem high. Their basis for comparison might be the low frequently undervalued reimbursement rates that they accept for their work from third-party payers for therapeutic medical services. But cosmetics is not therapeutics. It's a luxury service. In fact, taking similarities in operating time and requisite resources into consideration, cosmetic vaginal surgery fees are in the same range as most breast augmentation and liposuction procedures, and less than those typical of abdominoplasty, face lifts, and cosmetic dentistry. No talk about cosmetic gynecology would be complete without talking about David Matlock. David started out practicing Ob Gyn in Beverly Hills in the 1980s. He started offering vaginoplasties to enhance sex in a newspaper ad after a few patients who underwent colporrhaphies for gyn conditions mentioned that it had a positive effect on sex. He went to business school several years later and made this the focal point of a business school project. He trademarked his style of vaginoplasty and labiaplasty, then added the G-shot for the G-spot to round out his portfolio of cosmetic gyn services. Then he developed a franchise model for others to learn the procedures and perform the procedures using trademarked terminology. But what really departed from anything that had been done by anyone in medicine before was that he instituted a gag clause. He started this business in 2002 with heavy advertising in journals and then at meetings. Around the same time, cosmetic surgery exploded in popularity worldwide thanks to the introduction of botox, reality tv, a lax credit market and the birth of social media. Cosmetic gyn was all over the media even though in reality, the number of cosmetic gyn surgeries, even in David’s clinic didn’t approach the number of procedures performed for breast augmentation or liposuction in busy cosmetic practices including his own. Nonetheless, in 2007, ACOG, for the first time addressed cosmetic vaginal procedures by means of a Committee Opinion from the Committee on Gynecologic Practice targeted directly at David’s business. The committee which produced the opinion defines itself as a developer of state-of-the-art commentaries. The ACOG Committee on Gynecologic Practice produced 3 Opinions in 2007. As you would expect, they normally support their state-of-art opinions with references. As you can see, the first two had a total of 22 references combined, but this opinion only had one reference. They carefully crafted their document to identify all of Matlock's trademarked terminology without infringing upon the trademarks and incurring legal exposure. They stated that his terminology was unclear, they speculated as to what they thought the procedures might be, they speculated as to what they thought the complications might be based on their unreferenced assumptions, they filled it with innuendo. But most importantly, what they didn’t do was interview David. The ACOG motive for issuing an alarmist document lacking even the most basic review of relevant literature is unclear, but it does not appear that the motive was to produce a state-of-the-art commentary. It only has one reference. And what was this incredible reference... A paper that states that vulvar and vaginal dimensions vary. That’s it! Strangely enough, just one year later a non-physician from New Zealand submits a review article on cosmetic gyn and finds over 150 references many of which predated the ACOG opinion. The merit of this document needs to be understood for the piece of political propaganda that it represents. It has stood unchallenged long enough and it has never been a state-of-the-commentary on cosmetic vaginal surgery. I’m done talking about David & stirring up the pot. We need to stop ignoring people who request cosmetic gynecology services. We need to stop dismissing their concerns as trivial. We need to accept that there is nothing wrong with cosmetic surgery. We need to give realistic expectations of what cosmetic surgery can and cannot accomplish. END OF LECTURE Author's NoteI ended the lecture three slides short of the planned ending due to time constraints. The real ending was intended to evoke a strong and uncomfortable emotional response among audience members by challenging root values and the meaning of ethics. Think about them as the provider of the service, the choices you make & that society must make to justify the actions. Here are the slides:
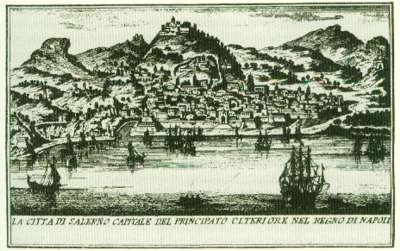
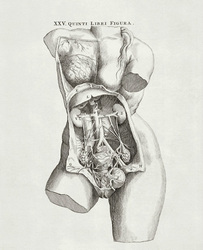
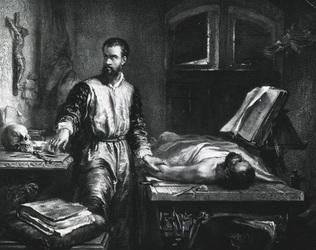
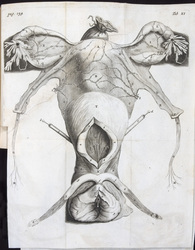
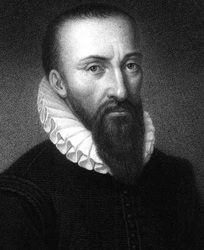
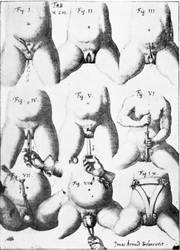
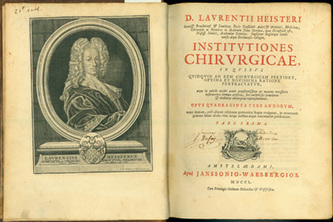
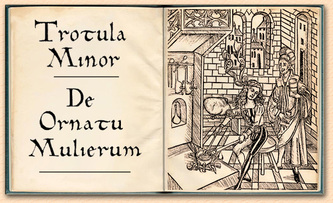
Vaginal rejuvenation, or tightening, is over one thousand years old, and it was conceived by women. As mentioned in Part I, the work of the female physician Trotula de Ruggiero of Salerno was published in 1050 AD under the title Treatments for Women. In this volume are five nonsurgical recipes for "restoring" virginity. The section opens as follows: A constrictive for the vagina, so that women may be found to be as though they were virgins, is made in this manner Renowned Medieval historian Monica Green who spent decades researching all extant versions of the Trotula ensemble and Salernan culture prior to her definitive translation opines: It may be that some of these constrictives were meant only to tighten the vagina to the enhance the friction of vaginal intercourse, not necessarily to produce a fake bloodflow of "defloration"; in other words, they may have been intended as aids to sexual pleasure within marriage. The Renaissance brought major advances in anatomic knowledge through cadaveric dissections best represented by Vesalius (1514-1564) at the University of Padua in De Humana Corporis Fabrica. Owing to the invention of the printing press, this knowledge became widely disseminated. However, little if any change in took place in gynecologic surgical technique or instrumentation from that of the Greco-Roman era . Nonetheless, celebrated French surgeon Ambroise Paré (1510-1590) in Gynaeciorium Physicus et Chirurgicus, then his pupil Jacques Guillemeau (1550-1612) in his 1609 text De la Grossesse et Accouchement des Femmes, were first to describe repairs of rectovaginal lacerations at childbirth. Spaniard Roderico a Castro (1546-1627) described clitoridectomy by a horse hair ligature tightened daily in Philosophiae Ac Medicinae Doctoris per Europum notissimi first published in 1604. The first illustration of excision for clitoral hypertrophy was provided by the German surgeon Johann Schultes (aka Scultetus 1595-1645) in Armamentarium Chirurgicum published posthumously in 1655. Pierre Dionis, a Parisian surgeon, described excision of the nymphae (labiaplasty) in his Cours d’opérations de chirurgie (1707) based on his work in the late 1600s in the court of Louis XIV. German military surgeon Lorenz Heister (1683-1758) described labia minoraplasty in full detail in his text, Institutiones Chirurgicae (1739), one of the most popular illustrated surgical texts of the eighteenth century: The nymphae in women are sometimes so large, as not only to hang without the labia pudenda, but also to prove troublesome to them in walking, sitting, and in their conjugal embraces; and may therefore require the surgeon’s assistance. The operator is therefore in the first place to lay the patient in a proper posture, and taking hold of the nymphae with his left hand, he is then to cut off so much of them with a pair of scissors in his right, as he shall judge necessary, taking care to have in readiness styptics for the haemorrhage, and medicines to prevent the patient from fainting. When the operation is over, the wound may be dressed with some vulnerary balsam, and healed without much difficulty in the common method. Key Points1. Vaginal rejuvenation, or tightening, is over one thousand years old, and it was conceived by women.
2. Clitoroplasty, in the Western world, was performed for appearance only through the eighteenth century. 3. Labiaplasty was an established treatment for both symptomatic and aesthetic concerns by the late seventeenth century. I can think of no finer way to inaugurate the ISCG Blog than to explore the history of cosmetic vaginal surgery. Where possible I have linked to online translations for reference and scholarship. Soranus of Ephesus, a Greek physician who practiced in Alexandria and later in Rome from the end of the first century to the beginning of the second century AD, provided the first written record of surgery performed on the female genitalia for cosmetic effect. In a 6th century Latin translation by Muscio of his 4-volume treatise entitled Gynaecology, he describes the excision of a hypertrophied clitoris for cosmetic reasons and to diminish excessive sexual stimulation. He credits the procedure to Philumenus (not the 3rd century Philumenos), one of his older Greek contemporaries: The patient was placed in a lithotomy position and held in place by able bodied assistants. The surgeon grasped the clitoris with broad toothed forceps and cut above the instrument...Bleeding was controlled by cold compresses soaked in vinegar and styptic powder. Philumenos of Alexandria, in the third century AD, described excision of the hypertrophied clitoris because it was considered "ugly and disgraceful." His work was abstracted by the Byzantine physician Aetios of Amida in his 4th century work Sixteen Books on Medicine. The practice of excising the nonhypertrophied clitoris originated in Egypt in an effort to prevent any desire for coitus in premarital girls and not out of any cosmetic motivation. In the seventh century AD, Paulos of Aegina, another Byzantine physician describes two distinct operations in his Medical Compendium in Seven Books. The first operation is his technique of excision of the hypertrophied clitoris, which he refers to as the nympha. The second operation is an excision of enlarged labia minora which he refers to as cauda pudendi or pudendal tail: The cauda is a fleshy excrescence arising from the mouth of the womb, and filling the female pudendum, sometimes even projecting externally like a tail; and it may be removed in the same manner as the nympha. The suturing of vaginal lacerations at childbirth forms the basis for all modern vaginoplasty techniques. The procedure was first described circa 1050 AD by a female physician, Trotula di Ruggiero of La Scuola Medica Salernitana, the first medical school in Europe. She wrote Treatments for Women as well as contributions to another work De Ornatu Mulierum (Women's Cosmetics) which, in addition to two other works written subsequently by other medieval physicians comprised the compendium commonly known as The Trotula. Key Points1. Cosmetic vaginal surgery can be traced back to the Greek physician Soranus of Ephesus, in first century AD.
2. Labiaplasty was first performed by the Greek physician Paulos of Aegina, in the seventh century AD. 3. The origins of vaginoplasty began with the female physician Trotula di Ruggiero of Salerno, in the 11th century. |
AuthorMarco A. Pelosi, III, MD, is a cosmetic gynecologist, surgeon, lecturer & cofounder of the ISCG. You may contact him directly at [email protected] Archives
April 2020
Categories
All
|
We are ISCG |
Get to Know Us |
Stay Connected |




































 RSS Feed
RSS Feed
