|
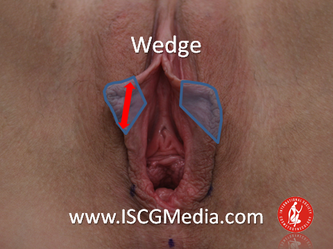
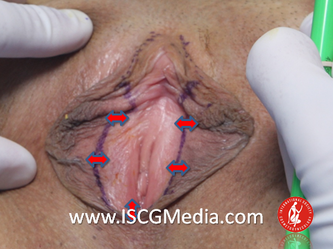
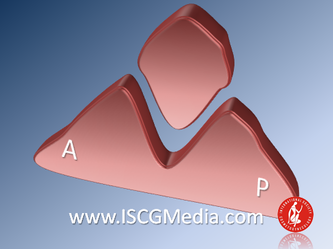
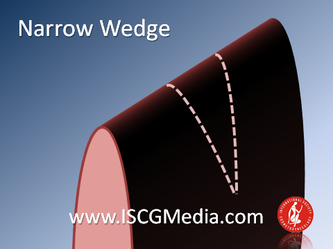
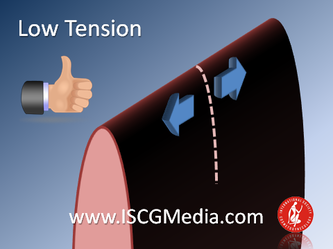
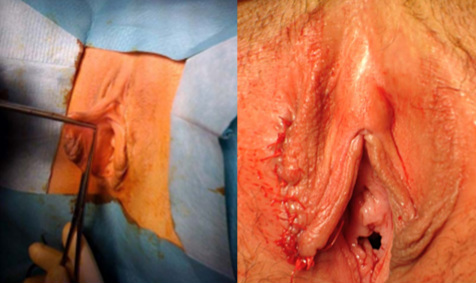
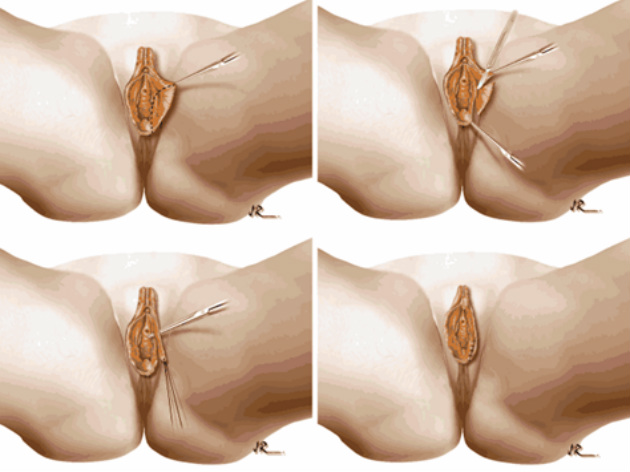
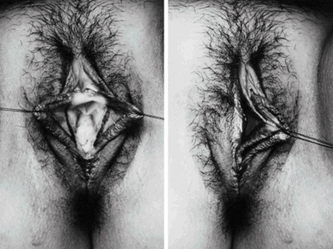
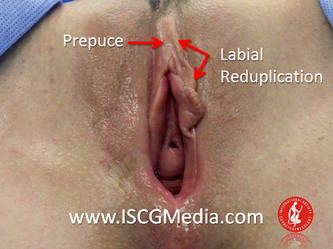
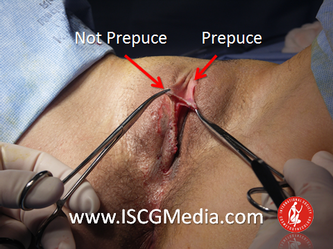
I wanted to share a small sample from an upcoming chapter entitled Cosmetogynecology Note: I took a few liberties with the official version of my work as it will appear in the published version to provide you, the blog reader, with some behind-the-scenes perspectives and anecdotal observations that I usually omit for both brevity and lack of published references from more "learned" discussions. Also, I have included images that exceed those of the to-be-published work because there are no restrictions on quantity here. Bon apetit!  Dr Shirith Sheth Dr Shirith Sheth Shirith S. Sheth, FRCOG Ad Eundem, FACOG (Hon), is an exquisitely skilled, renowned and celebrated gynecologic surgeon from Mumbai, India. He is also a good friend to my surgical team and an individual whom we see much too infrequently. Over a decade ago, we contributed chapters to his excellent book entitled Vaginal Hysterectomy which he co-edited with Dr. John Studd. Several months ago, Dr. Sheth decided that his masterpiece was due for an overhaul and asked if we would be so kind as to update our chapters. He also asked if there was "anything new" that might add to the appeal of the book. Ergo, a chapter on cosmetic gynecology, to be released early next year. We hope you'll like it. LABIA MINORAThe labia minora display a wide range of shapes, sizes, pigmentation and frequent asymmetry. Controlled precise resections are employed to reshape the labia and the skin around the clitoral hood. Some requests are purely cosmetic, others address pain or irritation associated with certain activities such as sex, horseback riding and other sports. Symmetry, balance and comfort are the most common reasons why women request cosmetic alterations of the labia minora. In some instances, treatment is unilateral. Two of these cases presented with complaints of traction pain with various activities. The other two simply disliked the appearance. Can you match the symptoms with the images? - of course not! Myriad techniques for labia minoraplasty abound. They can be categorized into three general groups: (1) linear excisions parallel to the labial edge, (2) wedge excisions perpendicular to the labial edge, and (3) partial-thickness excisions. All of these approaches have been described with variations on the shape and extent of the basic concepts. Linear Labia MinoraplastyModern linear excisions are radically evolved from the simple amputations of antiquity which were originally preferred for their speed in the pre-anesthetic era. The refined cosmetic approach involves a layer-by-layer contoured dissection with hemostatic adjuncts such as vasoconstrictor injections and frequently electrosurgical, radiofrequency or laser coagulation. Linear excisions offer the ability to remove and reshape the entire length and profile of the labial edge. They also allow for precise tension adjustments and typically yield a low-tension suture line and do not generate posterior traction on the clitoral frenulum. If there is a marked color discrepancy between lateral and medial labial skin, this style of labiaplasty may leave an unnatural color transition line along the new labial edge if an aggressive excision is performed. In a full-length excision, 3 to 4 small arterioles will be encountered and require surgical control. Wedge Labia MinoraplastyMarc Laufer (pictured), and William Galvin, pediatric gynecologists at Children's Hospital/ Brigham & Women's Hospital, Boston, Massachussetts, published a 2-case report introducing the wedge labiaplasty technique in 1995 (Adolescent and Pediatric Gynecology 1995;8:39-41). Three years later, Gary Alter, a plastic surgeon from Los Angeles, published a 4-case series introducing the wedge labiaplasty technique. (Annals of Plastic Surgery 1998;40:287-90). In fairness to Alter, I was unable to find Laufer's paper in any medical database using 2013 search technology with a copy of Laufer's paper right in front of me. So how did I find Laufer's obscure paper? He self-referenced it in a 2011 article on pediatric labiaplasty. Wedge excisions offer the ability to preserve the natural labial edge, but cannot reshape the full length of the labial margin. The approach was originally conceived in an effort to reduce scarring and discomfort associated with improperly performed linear excisions (Laufer 1995; Alter 1998). They are a reasonable option when the tissue targeted for excision is limited to a narrow segment of the labium. In a typical wedge excision, a single arteriole is encountered. Wedge excisions near the clitoris have a tendency to draw the frenulum and clitoral hood posteriorly. Attempts to extend the aesthetic reach of this style of labiaplasty by either wider wedging or creative flapping are met by an unacceptably high rate of either incisional dehiscence or tissue necrosis. Partial-Thickness Labia MinoraplastyPartial-thickness skin-only excisions of the labia minora have been proposed with the goal of preserving the labial edge. Two techniques have been described. One of these entails triangular epithelium-only excisions parallel to the long axis of the labium on the medial and again on the lateral aspects. The stroma and vascular supply are not disturbed (Choi et als.). A second approach consists of the resection of a skin-only wedge from the central portion of the labium and consistently leaves a thickened appearance. Clitoral HoodEssentially a component of the labia minora aesthetic unit, the clitoral hood (prepuce) varies greatly in anatomy. Frequently, one finds reduplication of the labia minora extending laterally or bilaterally parallel to the shaft of the clitoris. In other instances, the clitoral hood itself displays loose, redundant folds. Targeted, superficial direct excision of this redundant tissue is individualized. The best cosmetic results are achieved by maintaining suture lines parallel to the clitoral shaft. A cosmetic error, frequently seen with improperly designed linear excisions, is the abrupt termination of the labiaplasty scar at the clitoral hood, leaving a loose redundant mass of periclitoral skin. These require revisionary surgery to essentially complete the procedure. That's it!
If you want more, you'll have to buy the book or see me in person.
1 Comment
|
AuthorMarco A. Pelosi, III, MD, is a cosmetic gynecologist, surgeon, lecturer & cofounder of the ISCG. You may contact him directly at [email protected] Archives
April 2020
Categories
All
|
We are ISCG |
Get to Know Us |
Stay Connected |























 RSS Feed
RSS Feed
