|
This article was originally published on LinkedIn on December 28, 2019. and it was the transcript of a podcast on The Top Cosmetic Gynecologists released on December 26, 2019. The path of the righteous man is beset on all sides by the inequities of the selfish and the tyranny of evil men. Like that distorted passage that evokes the air of biblical authority from a version of Ezekiel 25:17 that never existed, today’s topic also focuses on a heavily twisted blend of fact and fantasy trying desperately to attain an air of unquestioned authority. A quest that will be stricken down here today. Wearing all of the the lipstick, so to speak, of an authoritative document from an otherwise reliable source, the uninitiated and the casual reader alike might miss the glaring nature of that which they might accidentally embrace. I’ve devoted this essay to the goal of ensuring that this does not happen. A Few Good TermsLet’s button down a few concepts central to our exposé first so that we can roll smoothly and logically. First, let’s define expertise, the state of being an expert of the principles and practice of a body of knowledge. What is an expert? The most common definition of an expert is a person who has a comprehensive and authoritative knowledge of or skill in a particular area. I think you have to have both. By way of example, Tiger Woods is an expert in golf. His coach is not. His coach is an expert in coaching golf, but not necessarily in the skill of actually swinging the clubs. A novice might even beat him. I think that’s a suitable definition of an expert and conveniently, it brings us to the concept of being authoritative. What does it mean to be authoritative? ...or to say that something or someone is authoritative? The most common definition of authoritative is the state of being able to be trusted as being accurate or true. In the legal world, authoritative takes on a slightly different meaning. When one states that a source is authoritative, they are saying that that source takes precedence over others. That’s why lawyers frequently trap those who are legally naïve to state that a given source is authoritative during a deposition. You see in law, the accuracy or the truth of the source don’t matter. What matters is that you said they were true. And if you assumed that a source was true today because it’s true most of the time on most matters on other days, you just turned something that wasn’t true and wasn’t accurate into something that can be used against you in a court of law as if it were true and accurate simply because you trusted them blindly today. Let’s leave the courtroom and visit the field of psychology for our third and final concept before we launch into main event: The Concept of the Halo Effect The Halo Effect is the tendency for positive impressions of a person, company, brand or product in one area to positively influence one's opinion or feelings in other areas. It is a type of cognitive bias. For the today’s purpose, we’re going to refine and sharpen our halo effect to mean that it is the tendency for anyone who is a committee member of a committee of an American college of obstetricians and gynecologists who is an expert in traditional OBGYN subject matter automatically to be thought of as an expert in cosmetic gynecology without training, education or experience in cosmetic gynecology. Let the Games BeginThere is a committee on gynecologic practice in an American college of obstetricians and gynecologists. This committee consists of 31 physicians and 5 allied health professionals who in part and in their self-described mission “develop state-of-the-art commentaries on gynecologic subjects related to clinical management as necessary.” The committee members undergo a personnel churn on a yearly basis for some members and on a longer basis for others. The topics on which they produce statements is dictated by others in the College hierarchy and the production of a statement is a year-long process with more than one in-person meeting of the entire group. I know this because I’ve been there and done that. Of these 36 people, all of whom are the finest people exemplary in their field, all of whom have devoted their careers to the promotion of women’s health, many of whom cater daily to the medical needs of women, many of whom are devoted to the education and development of future women’s healthcare professionals, none have any training, education or experience in cosmetic gynecology. I don’t state this casually. I checked and cross-referenced every single member of this committee against every commonly used term to identify procedures and services in the field of cosmetic gynecology. These people recently published an opinion on cosmetic gynecology entitled Committee Opinion: Female Genital Cosmetic Surgery that includes Recommendations and Conclusions. To summarize so far: A committee of non-experts in cosmetic gynecology From an American college of non-experts in cosmetic gynecology Published an opinion on cosmetic gynecology. Let that sink in... A committee of non-experts in cosmetic gynecology From an American college of non-experts in cosmetic gynecology Published an opinion on cosmetic gynecology devoid of expertise and put forth a series of recommendations and conclusions. Let's take a look at this document in detailLet’s dissect it. Let’s analyze it. And let’s see what type of statement has been concocted by these non-experts in cosmetic gynecology. We will tackle it from beginning to end. I will read sections of the text and give you my impressions at all relevant intervals. For ease of interpretation, I have placed the text from this document in italics for the remainder of this essay. Committee Opinion No. 795 Elective Female Genital Cosmetic Surgery ABSTRACT: “Female genital cosmetic surgery” is a broad term that comprises numerous procedures, including labiaplasty true, clitoral hood reduction true, hymenoplasty true, labia majora augmentation true, vaginoplasty and G-spot amplification. G-spot amplification is not a surgical procedure. Any expert in cosmetic gynecology knows this. Any novice in cosmetic gynecology knows this. Patients know this. So what’s G-spot amplification doing on a list of surgical procedures? There are only two possibilities: Either it was included out of sheer ignorance due to a total lack of experience with the topic of cosmetic gynecology or it was placed there deliberately for reasons unknown. To me, it wreaks of ignorance. Remember, this document is the product of 36 non-experts in cosmetic gynecology sitting around a table. Both patient interest in and performance of cosmetic genital procedures have increased during the past decade. Lack of published studies and standardized nomenclature related to female genital cosmetic surgical procedures and their outcomes translates to a lack of clear information on incidence and prevalence and limited data on risks and benefits. All True. Women should be informed about the lack of high-quality data that support the effectiveness of genital cosmetic surgical procedures and counseled about their potential complications, including pain, bleeding, infection, scarring, adhesions, altered sensation, dyspareunia, and need for reoperation. Sounds good right? It’s got that authoritative tone and a little bit of fear factor tossed in there. Well, not so fast. How do you measure the effectiveness of any cosmetic procedure? Breast? Nose? Cosmetic gyn or anything else? Simple. The patient is happy with her result. Her expectation was met. That can only be measured by asking the patient if she’s happy. If she’s unhappy it’s a total failure. Even if the result was technically perfect. And you can’t measure that with a number. The result is subjective. And subjective data is never high-quality data. It’s opinion all the way and that means that you will never be able to extract high quality data on the effectiveness of any cosmetic procedure Whether it’s breast, nose, cosmetic gyn, tummy tuck, facelift, liposuction or anything else. It’s always going to boil down to patient satisfaction. Any expert in cosmetic gynecology or cosmetic surgery in general knows this. Furthermore, even if we had the highest quality level 1 evidence on the subjective endpoint of making women happy in some imaginary world, it’s non-transferable. No two women have the same expectation of what will or won’t make them happy. Just because 99 percent of women were happy with procedure X doesn’t mean that the next patient that walks through the door will be happy. Setting the expectation, which wasn’t addressed all in this document, would be central to this process. Let’s take a look at the second part of the statement that women should be counseled about the potential complications. Yes. It’s always a good idea to review the risks of a procedure any procedure with the patient. It’s part of any informed consent process anywhere in the world. However and apparently, when they talk about potential complications, they are no longer concerned about the lack of high quality data on potential complications. “Potential complications” gets a free ride on that because it’s negative. It’s anti cosmetic surgery. It’s there to create fear. Now, don’t get me wrong, these potential complications are real. But they are extremely rare in the hands of trained, educated and experienced cosmetic gynecologists. So if you really want to make a statement that doesn’t sound like fake news, you need to wake up to the reality that there is an entire world of expert cosmetic gynecologists who treat women every day and rarely see these issues. I counsel my patients that these issues that non-experts bark about are definitely a real and present danger in the hands of nonexperts, but not mine where they are rare. And I have over two decades of experience to show for it. And so do my expert colleagues. But we weren’t consulted. And I know that they know who I am, where I am, and how to reach me and my expert colleagues. It is very unusual that no experts in cosmetic gynecology were recruited as subject matter experts to be a part of this committee. I can’t think of any industry or professional endeavor in which bringing in an expert wouldn’t be viewed as essential to producing a professional level statement. Obstetrician–gynecologists should have sufficient training to recognize women with sexual function disorders as well as those with depression, anxiety, and other psychiatric conditions. Individuals should be assessed, if indicated, for body dysmorphic disorder. In women who have suspected psychological concerns, a referral for evaluation should occur before considering surgery. This is an excellent recommendation. I would add, from my vast experience, that it is common for patients with body dysmorphic disorders to seek out providers of cosmetic surgery and that the prevalence of such patients is higher than the prevalence of this condition in the general population. As for all procedures, obstetrician–gynecologists who perform genital cosmetic surgical procedures should inform prospective patients about their experience and surgical outcomes. YES! I addressed this above. The surgical experience and outcomes of the individual surgeon is the only thing that matters in the individual case. My expertise is not your expertise. My excellent results don’t imply that others will necessarily have similar results unless they practice at a similar level with similar techniques. Patients should be made aware that surgery or procedures to alter sexual appearance or function are not medically indicated, pose substantial risk, and their safety and effectiveness have not been established. (excluding procedures performed for clinical indications, such as clinically diagnosed female sexual dysfunction, pain with intercourse, interference in athletic activities, previous obstetric or straddle injury, reversing female genital cutting, vaginal prolapse, incontinence, or gender affirmation surgery). This is the craziest statement of all. When I titled this essay Lipstick on a Pig, this is the Pig. There are two huge glaring warts on this pig. The first is a fatal flaw in logic: the statement says that all things being equal, the safety and effectiveness of a surgical procedure hinges on whether it is clinically indicated or not based on their desperate list of “clinical indications” that seems to have been jammed into the document at the last minute. By this twisted reasoning, if a pair of identical twins underwent labiaplasty – one sister for pain and the other for cosmetic effect, one would be at higher risk for complications than the other. That is insanity. I’m not making this up. I’m reading it from this “state-of-the-art commentary”. But that’s not all. When they provide a list of procedures that are excluded from attack because they are clinically indicated, they don’t provide ANY clinical data that their list of of procedures that are excluded from attack are safe or effective. They’re asking you to give them a free pass. The second wart on this pig, is their statement that these procedures pose not just a risk, but rather a substantial risk. They used the word substantial. Substantial is not a benign word. Substantial is a very dangerous word. Substantial means large. And large speaks to data. And when there is no data anywhere in this document or in the references of this document that shows large risk associated with cosmetic surgery …and you know this, then you are telling me that you don’t really care about data. You are showing me that you have an agenda and that you care more about that agenda than you care about data. And if you produce a pernicious, mendacious unsubstantiated declaration in the age of transparency, you can’t hide. I’ve seen the credentials of every single person on this committee. I know what they know and I know what they don’t know. I know when they’re telling the truth and I know when they’re…let’s call it speculating to be polite. Recommendations and Conclusions The American College of Obstetricians and Gynecologists makes the following recommendations and conclusions regarding the use of and indications for female genital cosmetic surgery. Remember, these people are not experts in cosmetic gynecology. They have no training, no education and no experience in this field. • Patients should be made aware that surgery or procedures to alter sexual appearance or function (excluding procedures performed for clinical indications, such as clinically diagnosed female sexual dysfunction, pain with intercourse, interference in athletic activities, previous obstetric or straddle injury, reversing female genital cutting, vaginal prolapse, incontinence, or gender affirmation surgery) are not medically indicated, pose substantial risk, and their safety and effectiveness have not been established. We just discussed the illogic of this statement a few minutes ago. Cosmetic surgery is never medically indicated, but you can’t use the word Substantial when talking about the risk if you don’t have any data to prove it. From the tone you would think that there’s a pile of burning bodies and a wake of devastation as if a Mongol Horde had swept through the female population. And what’s going to happen if we don’t nip this nonsense in the bud is that those who don’t know a thing about cosmetic gynecology, those who assume that everything that comes of out the American College of Non-Experts in Cosmetic Gynecology is automatically correct are going to start to believe it. And when they start to believe it, you’re going to have to stand your ground and defend your livelihood from these misguided souls screaming mindlessly that cosmetic gynecology carries substantial risks. So if you value your business, get out there and start poking holes in these weak arguments fiercely and frequently. I’m giving you fair warning. You cannot stand by and watch. You must take control. • Women should be informed about the lack of high-quality data that support the effectiveness of genital cosmetic surgical procedures and counseled about their potential complications, including pain, bleeding, infection, scarring, adhesions, altered sensation, dyspareunia, and need for reoperation. We covered this already too. When effectiveness is measured subjectively, when it is the opinion of the patient whether her expectation was met, you will never have high quality data. That being the case, the bar for effectiveness for cosmetic gyn surgery is the same as that for breast augmentation, face lifts, rhinoplasty, tummy tucks and body contouring and the rest of the medical world doesn’t have a problem with that. We also discussed the association between expertise and a low risk of complications and a lack of expertise and a high risk of complications. • Obstetrician–gynecologists should have sufficient training to recognize women with sexual function disorders as well as those with depression, anxiety, and other psychiatric conditions. Individuals should be assessed, if indicated, for body dysmorphic disorder. In women who have suspected psychological concerns, a referral for evaluation should occur before considering surgery. This is true. It’s one of the few recommendations that’s grounded in reality and it is extremely important to keep a sharp eye out for those who have mental issues. • In responding to a patient’s concern about the appearance of her external genitalia, the obstetrician–gynecologist can reassure her that the size, shape, and color of the external genitalia vary considerably from woman to woman. These variations are further modified by pubertal maturity, aging, anatomic changes resulting from childbirth, and atrophic changes associated with menopause or hypoestrogenism, or both. I don’t know where they’re going with this here. Telling a woman who seeks out a cosmetic procedure that she’s normal makes sense if she’s doing it because she thinks it’s abnormal, but that’s really something in the psychological screening process. Almost all patients seeking cosmetic procedures have normal anatomy whether it’s cosmetic gyn, breast augmentation, facelifts, tummy tucks, or anything else. But having normal anatomy is not a reason enough to decline the request unless the request cannot be performed for technical reasons related to the specifics of her anatomy. Inconveniently true is the fact that tubal ligations, circumcisions and abortions are routinely performed on normal anatomy by members of the Committee. • As for all procedures, obstetrician–gynecologists who perform genital cosmetic surgical procedures should inform prospective patients about their experience and surgical outcomes. This is a statement that we addressed previously and that is certainly valid. • Advertisements in any media must be accurate and not misleading or deceptive. There’s nothing wrong with calling for truth in advertising, but this advice should apply equally to anything and everything in the field of obstetrics and gynecology. “Rebranding” existing surgical procedures (many of which are similar to, if not the same as, the traditional anterior and posterior colporrhaphy) and marketing them as new cosmetic vaginal procedures is misleading. If I were to rebrand a traditional anterior or posterior colporrhaphy as a procedure to tighten the vagina – a vaginoplasty, I – one of the world’s experts in vaginoplasty - would not achieve a tighter vagina. Many of the patients that I operate for vaginal tightening have had traditional anterior and posterior colporrhaphies and they come to me and my expert colleagues precisely because we use techniques that are distinct from these procedures. They might address the same anatomy, they might involve similar dissections and similar tools, but they are miles apart in both intent and effect. Of course, a committee of non-experts wouldn’t know that. Background Female genital cosmetic surgery, when referred to in this Committee Opinion, is defined as the surgical alteration of the vulvovaginal anatomy intended for cosmesis in women who have no apparent structural or functional abnormality. Genital cosmetic surgery will not refer to procedures performed for clinical indications (eg, clinically diagnosed female sexual dysfunction, pain with intercourse, interference in athletic activities, previous obstetric or straddle injury, reversing female genital cutting, vaginal prolapse, incontinence, or gender affirmation surgery). The goals of this Committee Opinion are to provide the following three items: 1) potential reasons for the increase in the number of cosmetic genital surgical procedures; 2) a brief overview of cosmetic vaginal procedures and outcomes data associated with them; and 3) an opinion on their use for the sole purposes of cosmesis, sexual function augmentation, or both. This Committee Opinion has been updated to include new data on elective female genital cosmetic procedures and their outcomes, as well as guidance on patient counseling. For guidance on labial surgery in adolescents, see Committee Opinion No. 686, Breast and Labial Surgery in Adolescents (1). Both patient interest in and performance of cosmetic genital procedures have increased during the past decade. For example, labiaplasty rates in the United States increased more than 50% between 2014 and 2018 (2). The next statement is a paragraph that starts with a false statement: At the same time, ethical and, more recently, safety concerns have been raised about the performance of cosmetic genital surgery. The reason that it’s false is that ethical and safety concerns about cosmetic genital surgery have NOT recently been raised. Their attempt to support this statement is also false. They say the following: In July 2018, the U.S. Food and Drug Administration (FDA) issued a warning against the use of energy-based devices (most commonly, radiofrequency or laser) outside of standardized research protocols for cosmetic vaginal procedures or vaginal “rejuvenation,” citing their potential for serious adverse events, including vaginal burns, scarring, pain during sexual intercourse, and recurring or chronic pain (3). That statement is a misquote of the actual FDA statement on which I wrote an in depth LinkedIn article last year when it first came out. They are trying to gaslight the reader – to mischaracterize past events to suit an ulterior purpose. The real FDA statement mentioned nothing about “standardized research protocols” or any language to that effect. The real FDA statement was directed at inappropriate marketing by the medical industry and not at clinicians. The real FDA statement said nothing about cosmetic genital surgery. The entire statement was about NON-surgical energy based devices for NON-surgical procedures. So the last place that it belongs is in document about surgical procedures. Any expert in cosmetic gynecology would know this. Potential Reasons for Increased Interest in Genital Cosmetic Surgery Shaving, waxing, electrolysis, and laser removal of pubic hair may allow a better view of the external genitalia for both women and their partners. In a cross-sectional study of more than 2,400 women aged 18–68 years living in the United States, 79% had partially or totally removed their pubic hair or were hair-free in the past month (4). One consequence of this procedure may be to draw more attention to asymmetries and differences in the external genitalia, potentially contributing to an increased desire for surgical alteration (5). I agree with this completely. It’s a change in the culture that started sometime in the 1990s and is currently the norm. Every gynecologist that I know say the same the thing. The perception of having aesthetically inferior external genitalia, augmented by the internet, online pornography, and other media sources, may drive women to seek surgical alteration (6). I pulled this reference. It was a review of 5 papers from outside the US from 2010-2012. Nowhere in this reference is the term “aesthetically inferior” used. The term “aesthetically unpleasing” is used instead. It’s significant. Also significant is that this paper only looked at content on a few foreign websites and nowhere in this paper did they ever collect or seek to collect any data on whether these websites had any effect at all on driving women to seek anything. For the record, the patients who seek me out for labiaplasty and other aesthetic procedures don’t come in because they feel inferior. They either personally dislike their appearance or feel physical discomfort. Women who explore cosmetic surgery often turn to internet searches. This should shock no one. We live in the age of internet searches for everything. I do it , you do it, it’s the world we live in. This is particularly important because the internet may be their only source of information (6). There is nothing in this reference that supports this statement. It was an analysis of websites not a survey of patients as to where they get their information. So it’s an opinion, but it’s presented as fact and that’s not being transparent. Also, it’s about to be contradicted in a the next section of the document by their next reference. A systematic review of online content that promoted female genital cosmetic surgery found that sites that promoted cosmetic genital surgery regularly described the wide variation of normal vulvar appearance as unnatural or diseased and implied that variation beyond the prepubescent-looking vulva (eg, no visible labia minora, narrow vaginal opening) results in distress and sexual dysfunction (6). This is reference #6 again which was a study of 5 papers covering a handful of websites of which were outside the USA (UK, Netherlands, Nigeria, Australia) In a cross-sectional survey of 395 participants, older women (45–72 years of age) were more likely to consider cosmetic genital surgery than a cohort of younger women (18–44 years) (7); this is not surprising given the societal emphasis on reversing the effects of normal aging. I pulled this reference too. And I found a few interesting things: First, the survey wasn’t validated. That means we can’t be sure that the women understood the questions adequately to give reliable answers. Second, and case in point, the question in the survey that asked about considering cosmetic surgery didn’t specify that it had to be genital surgery as our committee statement is trying to imply. Third, over 90 percent of all of the women in the study thought their vulva was normal. Finally, the women in this study said they got the majority of their information about the appearance of their vulva from their doctor #1 and women's magazines and anatomy books and not from the internet. There’s your contradiction to what was said previously when they said women get their information on this topic exclusively from the internet. I guess they didn’t expect the reader to check the references. In a prospective study of 33 women who sought labial reduction surgery at a London gynecology clinic, dissatisfaction with appearance was most commonly reported. For the entire cohort, however, the dimensions of the labia minora measured within the range of typical variability (8). We’ve already stated that cosmetic surgery is almost always done upon normal anatomy and explained the hypocrisy that exists in singling out surgery on this normal anatomy while ignoring cosmetic surgery performed on other normal anatomy elsewhere on the body and gynecologic surgery such as abortions and tubal ligations performed in the pelvis. Of equal importance are marketing claims that genital cosmetic surgery treats cosmetic and functional issues and enhances sexual satisfaction. Well in the case of vaginoplasty to correct vaginal laxity it certainly does and that’s the only surgical procedure aimed at improving sexual function. Again, anyone with experience in cosmetic gynecology knows this. Much of the increase in popularity seen in vulvovaginal procedures for nonmedical indications is associated with the success of direct-to-consumer marketing in the 1990s (9, 10). They reference this statement with a couple of poorly written papers written by anti-cosmetic surgery proponents with a stated radical agenda. In 2013, the Royal College of Obstetricians and Gynaecologists recommended, and the American College of Obstetricians and Gynecologists agrees, that women should be given accurate information about normal variations in genital anatomy and that advertisement of female genital cosmetic surgery should not mislead women on what is considered to be normal or what is possible with surgery (11). Characterizing normal anatomic variation as necessitating medical intervention exposes otherwise healthy women to unnecessary surgery with the potential for serious complications. This is all good and well despite their lack of expertise on cosmetic gynecology, but they miss the point completely that cosmetic surgery is always a choice and never a necessity. Additionally, industry-generated conditions and diagnoses, where a proprietary device is deceptively marketed as a proven treatment, are concerning (12, 13). This sentence is another reference to the FDA’s critique of the medical device industry on the marketing of nonsurgical devices for nonsurgical procedures. This entire article is supposed to be about surgery and this snippet of information has nothing to do with surgery. Outcomes of Cosmetic Gynecology Surgery “Female genital cosmetic surgery” is a broad term that comprises numerous procedures, including labiaplasty, clitoral hood reduction, hymenoplasty, labia majora augmentation, vaginoplasty, and G-spot amplification; I mentioned much earlier that G spot amplification is not a surgical procedure and that only someone with a complete lack of knowledge in cosmetic gynecology would not know this. Then they ask you to see Table 1 for descriptions of surgical techniques and complications. Putting bad information into a table makes it look pretty, but it doesn’t magically turn it into better information. Aside from labiaplasty, it is difficult to know how often these procedures are being performed. Lack of published studies and standardized nomenclature related to female genital cosmetic surgical procedures and their outcomes translates to a lack of clear information on incidence and prevalence and limited data on risks and benefits. In general, the safety and effectiveness of these elective procedures have not been well documented, and evidence largely is restricted to clinical case reports and retrospective studies. Measures used to assess outcomes, such as patient questionnaires, are rarely comparable across studies, and follow-up rates vary widely (14). All of this is true and the problem with nomenclature is something that I have addressed frequently in lectures and most recently on episode 20 of this podcast in the context of vaginal laxity. Reports of patient satisfaction should not serve as evidence that these procedures are clinically effective (15). Actually, for cosmetic procedures, patient satisfaction is the only outcome that matters and that can only be measured by questionnaires. Labiaplasty is the most commonly performed cosmetic genital surgical procedure, and a variety of techniques have been described (Table 1). Clitoral hood reduction frequently is performed at the time of labiaplasty to reduce the occurrence of clitoral hood sagging after labiaplasty alone. In a multicenter retrospective cohort study of 258 women who underwent 341 cosmetic genital procedures, 177 underwent labiaplasty, clitoral hood reduction, or both (16). Although this study reported high patient satisfaction and enhancement in sexual function, these results should be interpreted with extreme caution given the lack of a comparison group and use of poorly constructed questionnaires, none of which were validated. Although validated scales were used in the same author’s 2016 prospective cohort case-controlled study of 120 individuals, only 54% of the women having genital cosmetic surgery chose to complete the scale at entry, versus 76% of controls (17). Even with greater use of validated scales in more recent literature, comparability remains difficult with the rare use of the same scale in more than one study. Do you see the game they’re playing here: When you give them data, and it supports that women are satisfied with cosmetic gyn surgery, they tell you that the data is no good When they find even the weakest shred of even a hint of unsubstantiated and sometimes even imagined negativity toward cosmetic gyn surgery, they give it massive importance and drama that it doesn’t deserve and start throwing around phrases like substantial risk. The next item in the article is Table 1 entitled Cosmetic Genital Procedures The bottom half of the table lists nonsurgical procedures and doesn’t belong in an article on surgery.
There is a column entitled Reported OR Potential Complications Do you know the difference in meaning between the word "reported" and the word "potential"? I do. Reported means real and potential means possible and possible can mean imaginary and never happened And if you title a column Reported OR Potential, you can stuff whatever you want underneath it even if everything in that column is imaginary and never happened. Pretty convenient stuff. Procedures that focus on the vaginal canal are marketed to improve sexual function. One of the most controversial female genital cosmetic surgical procedures, vaginal “rejuvenation,” is a proprietary term meant to encompass perineoplasty, vaginoplasty, or both, as a technique to reduce the diameter of the vagina, strengthen the perineal body, and enhance sexual function (18). The surgical technique used is very similar, if not identical, to anterior or posterior colporrhaphy and often is combined with perineoplasty. This is a twisted statement full of contradictions and the authors being non-experts in cosmetic gynecology are confused. First, the only controversy surrounding the term vaginal rejuvenation is its meaning. It is vague and has no meaning. Even experts in cosmetic gynecology don’t use this term to refer to a specific operation. Second, the authors seem to be speaking about vaginoplasty – the vaginal tightening surgery - in their critique on its ability to improve sexual function which is a poor choice of words on their part. The function of sex is reproduction. A better phrase, one that an expert would use, would be to improve sexual friction by reducing laxity. Third, they think that a vaginoplasty of this type is “very similar, if not identical to anterior and posterior colporrhaphy”. This statement makes me laugh the loudest because only someone who has never seen a vaginoplasty would ever say that. And anyone who has ever tried to tighten a vagina with a standard AP repair would never have a happy patient if they tried. I know this, I fix the sequelae of these misguided attempts by non-experts regularly. Another method for treating vaginal laxity, described as vaginal rugation restoration, involves use of the CO2 laser to create vaginal rugae in women in whom absent or decreased vaginal rugation has been diagnosed. Scant information on the outcomes (risks and benefits) of laser assistance, rugation restoration, or G-spot amplification exists in the peer-reviewed literature, and the published data are mostly restricted to expert opinion, case reports, or small case series (19). A 2012 prospective observational study of vaginal rugation restoration included only 10 women who underwent the procedure, making it difficult to draw conclusions (20). I don’t know why they decided to give vaginal rugation so much space in this article. I know the long-retired author of the only two papers ever written on this, I know the papers, and I know that very very few people use this technique and those that do use it don’t use it as a treatment for vaginal laxity. So if they wish to attack vaginal rugation, they are attacking a handful of people doing a handful of procedures that don’t really represent the common procedures of cosmetic gynecology. Once again, any expert in cosmetic gynecology knows this. The next statement is one we threw out already because it’s about nonsurgical energy based devices and the authors didn’t know that these are nonsurgical treatments: The FDA’s 2018 Safety Communication warned against the use of energy-based devices (commonly radiofrequency or laser) to perform vaginal "rejuvenation," cosmetic vaginal procedures, or nonsurgical vaginal procedures to treat symptoms related to menopause, urinary incontinence, or sexual function (3). Prospective studies that used validated measures of quality of life, body image, and sexual function are needed to understand the true benefits and harms of these procedures. That’s a great idea. Research should be conducted by those without a financial interest in the outcomes (14). Patient Counseling Understanding a woman’s motivation for cosmetic surgery requires careful and sensitive exploration to ensure her autonomy and rule out the possibility of coercion or exploitation by another person, such as a partner or family member. See ACOG Committee Opinions No. 578, Elective Surgery and Patient Choice, No. 390, Ethical Decision Making in Obstetrics and Gynecology, and No. 787, Human Trafficking (21-23). Labiaplasty in girls younger than 18 years should be considered only in those with significant congenital malformation, or persistent symptoms that the physician believes are caused directly by labial anatomy, or both. Surgical alteration of the labia that is not necessary to the health of the patient, who is younger than 18 years, is a violation of federal criminal law (24) (Box 1). At least one half of the states also have laws criminalizing labiaplasty under certain circumstances, and some of these laws apply to minors and adults. Obstetrician–gynecologists should be aware of federal and state laws that affect this and similar procedures in adolescents (1) and adults. Now, this is a cheap scare tactic placed here to give the impression that you're going to go to jail if you perform a labiaplasty. The laws that are on the books are speaking to female circumcision, infibulation, and ritualistic practices done against a person's will outside of legitimate medicine. They are not targeting labiaplasties and the majority of labiaplasties are not done in the pediatric population. It's an insignificant point that they're trying to make as if the surgeon is going to be criminalized for doing these procedures. Any lawyer will tell you this is nonsense. Obstetrician–gynecologists should have sufficient training to recognize women with sexual function disorders as well as those with depression, anxiety, and other psychiatric conditions. Individuals should be assessed, if indicated, for body dysmorphic disorder, criteria for which, according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, include a preoccupation with an imagined physical defect or exaggerated concern about a physical defect that would not be apparent to the casual observer, or a history of repetitive or obsessive behaviors (such as repeated examination or attempts to conceal the flaw, or continually seeking reassurance from others) (25, 26). In women who have suspected psychological concerns, a referral for evaluation should occur before considering surgery (27). These points were discussed earlier and require no additional commentary. They are valid. In responding to a patient’s concern about the appearance of her external genitalia, the obstetrician–gynecologist can reassure her that the size, shape, and color of the external genitalia vary considerably from woman to woman. These variations are further modified by pubertal maturity, aging, anatomic changes resulting from childbirth, and atrophic changes associated with menopause or hypoestrogenism, or both. Although labia minora longer than 30–40 mm is currently marketed as hypertrophic, in a study of 657 adolescent and adult females, the mean length of the labia minora (measured from clitoris to the lower margin of the labia) exceeded that estimate in more than 50% of the individuals (28). Measurements of the external genitalia must be interpreted on an individual basis, and age-related differences in the length of the labia minora vary widely (28). Table 2 provides information on the variability of female genitalia that can be used to counsel patients; however, the values should not be used to determine surgical appropriateness. Although patients often believe female genital cosmetic surgery will improve sexual function, current evidence does not support improvement in body image, libido, or sexual satisfaction. Concerns regarding sexual satisfaction may be addressed by careful evaluation for any sexual dysfunction, relationship issues, and an exploration of nonsurgical interventions, including counseling. For more information, see Practice Bulletin No. 213, Female Sexual Dysfunction (29). This entire section is an attempt to convince you to convince the patient out of having surgery for their own aesthetic concerns if their anatomy is normal. This is absurd because you wouldn't do this to someone who wanted a breast augmentation, a nose job, or any other cosmetic procedure. It is important to review patients’ expectations about the results of surgical intervention. Women should be informed about the lack of high-quality data that support the effectiveness of genital cosmetic surgical procedures and counseled about their potential complications, including pain, bleeding, infection, scarring, adhesions, altered sensation, dyspareunia, and need for reoperation. The possibility of dissatisfaction with cosmetic results, including potential adverse effects on sexual function, also should be discussed. A focus on patient expectations is critical to the success of any cosmetic procedure. If it's realistic and you can achieve it, the patient will be happy. However, if it's unrealistic, you're going to have a problem, she's going to have a problem, and you're never going to be able to achieve an acceptable result with an unrealistic patient. As for all procedures, obstetrician–gynecologists who perform genital cosmetic surgical procedures should inform prospective patients about their experience and surgical outcomes. Advertisements in any media must be accurate and not misleading or deceptive (30). “Rebranding” existing surgical procedures (many of which are similar to, if not the same as, the traditional anterior and posterior colporrhaphy) and marketing them as new cosmetic vaginal procedures is misleading. This entire rebranding concern is a misconception on the part of the authors because they know nothing about the nature of the cosmetic procedures. They seem to think that we are taking standard gynecologic operations, calling them cosmetic procedures, and then proceeding with traditional operations which is clearly not the case. Training Obstetrician–gynecologists who perform cosmetic procedures should be adequately trained, experienced, and clinically competent to perform the procedure (31). Extensive familiarity with appearance and function, as well as the ability to manage complications, are expected from obstetrician–gynecologists who perform these procedures. This was my favorite section and, in my opinion, the only thing of value in the entire document. The points made are obvious, but it would have been much better if they consulted with experts who could have given further guidance on how training and education and experience is obtained in light of the fact that the American College of Obstetricians and Gynecologists doesn't have that ability. Conclusion Obstetrician–gynecologists may receive requests from adolescents and adults for cosmetic genital surgery. For those choosing to provide cosmetic services, patient counseling (including definitions of normal range of anatomy and sexual function), shared decision making, and informed consent are paramount. Patients should be made aware that surgery or procedures to alter sexual appearance or function (excluding procedures performed for clinical indications, such as clinically diagnosed female sexual dysfunction, pain with intercourse, interference in athletic activities, previous obstetric or straddle injury, reversing female genital cutting, vaginal prolapse, incontinence, or gender affirmation surgery) are not medically indicated, pose substantial risk, and their safety and effectiveness have not been established. So there you have it, an in depth analysis of the latest “state-of-the-art” opinion written by a group with no experience in cosmetic gynecology. Judging by the fact that their first and only previous publication on the topic happened over 12 years ago, and that contemporary cosmetic gynecology has been around for over 20 years and is now a growing field globally, one would not be out of place in characterizing their behavior as reactive. Reactive as in “devoid of innovation”. Reactive as in full of agenda. A pernicious agenda. Clearly, they do not have their finger on the pulse of the state of the art. One should concerned, seriously concerned whenever an entity with a reputation for expertise in one area, with a reputation for publishing quality information goes off-brand off-the-rails and off-message on a poorly constructed alarmist rant about a topic on which they lack expertise. I hope you feel empowered and enlightened. ____________________________________ I'm most easily reached at DrMarcoPelosi.com
2 Comments
Cristo Papasakelariou MD, master pelvic surgeon from Houston, Texas, reviews the principles and demonstrates the surgical approaches to rectovaginal fistula repair. A great review for all cosmetic gynecologists from the ISCG archives. Recorded September 29, 2011, at the ISCG World Congress of Cosmetic Gynecology, Las Vegas, Nevada.
If you like this, check out all our World Congress lectures, conferences and congresses online here: https://vimeo.com/iscg/vod_pages
Dr Marco Pelosi III speaks to RealSelf about vaginoplasty with Dr Michelle Owens re-enacting the role of the interviewer. The article is geared to patient-centric concerns.
Just as the physically disabled adjust their mental processes to accomplish tasks designed for the typical human "package", so too must the 21st century surgeon adapt their thought patterns to evolve beyond the limitations of operations designed when the Enhanced Surgeon did not exist.
Tranexamic acid is the latest adjunct in cosmetic surgery for the reduction of bleeding, bruising, and postoperative swelling. Popular in the oral form (Lysteda) as a treatment for heavy menses since the 1980s, and the intravenous form (Cyklokapron) in cardiovascular and orthopedic surgery for the control of surgical hemorrhage for decades, it has also been used effectively by direct application to the surgical field by irrigation, soaked pledgets and tissue injection in hair transplantation and various aesthetic procedures of the face, breasts, and abdomen including liposuction. We have been using topical tranexamic acid in blephoroplasty, breast augmentation, abdominoplasty, liposuction, and abdominoplasty, and vaginoplasty for the past year with similar positive findings to those of recent authors. There is no precedent in vaginoplasty to the best of our knowledge. How we use tranexamic acid in cosmetic gynecologyA wide range of effective dosages for topical tranexamic acid is reported in the literature. Our most common application is in liposuction and the dosage we have been using for this procedure is 500mg tranexamic acid per liter of tumescent local anesthesia (TLA). We have used the same dose for all other applications including vaginoplasty. The method of topical application has been direct tissue injection at the time of local anesthesia infiltration and TLA-soaked surgical sponges. In the vaginoplasty example above, the right sided puborectalis muscle (medial border inked) is about to be injected with Tranexamic-TLA in preparation for levatorplasty. A midline pleated rectocele repair has been completed and the suture line is obvious centrally. Notice the excellent hemostasis of the entire field despite the extent of the dissection. Same operation after completion of a three-layer continuous levatorplasty. There is no bleeding from the puborectalis suture line. This means less postoperative swelling, inflammation and discomfort. Same operation at final stage (perineal reconstruction) showing hemostasis of the deep transverse perineal muscles (inked), superfical perineal muscles, and bulbocavernosus. The surgical sponge in the vaginal canal is serving as a temporary scaffolding for contour adjustment purposes, not for hemostasis. What precautions need to be taken when using tranexamic acid?Tranexamic acid is excreted through the kidneys. Patients must have normal renal function. Also, the concomitant use of oral contraceptives or a history of thromboembolic disease are contraindications to the use of tranexamic acid. The use of tranexamic acid has not been found to increase the surgical risk of thrombembolic disease. How does tranexamic acid work?This post was written as a practice pearl, recipe-style. You can delve into the mechanisms of action of tranexamic acid here. In brief, tranexamic acid keeps newly-formed blood clots from being broken down (fibrinolysis) by inhibiting plasmin.
They say levatorplasty is wrong. They say levatorplasty causes painful sex. They point to ancient literature and say, "there's the proof". They write new articles referencing the ancient literature and say, "look, there's more proof - it's in the references". I say they're wrong. Not about the accuracy of what they referenced. I've read the ancient literature, the modern literature, and everything in between. I've been performing levatorplasties for over two decades. My patients aren't experiencing the painful sex that my contemporaries have referenced and the Ancients have described. What's going on here? A review of the history of levatorplasty indicates clearly that their levatorplasty and my levatorplasty are not the same. A review of the ancient "proof" of levatorplasty-induced sexual pain (dyspareunia) reveals that these procedures were overaggressive in certain respects and incomplete in others. For the uninitiated, levatorplasty or more accurately, anterior levatorplasty is the practice of suturing the medial-most portion of the levator ani fibers (a section of the muscle called the puborectalis) immediately proximal to the anal sphincters across the midline and advancing this plication proximally, This is usually done through a perineal incision extended to the posterior vaginal wall. The practice of levatorplasty was introduced by Robert Ziegenspeck of Germany in 1900. To understand the problem with the "wrong" techniques of levatorplasty, we need to go back one hundred years ago and examine the work of Arnold Sturmdorf: In 1919, the influential and innovative Arnold Sturmdorf of New York, published and illustrated his technique of levatorplasty in his book, Gynoplastic Technology. His approach to muscle plication was incorporated by almost all techniques that followed. Sturmdorf's levator "myorrhaphy" begins with a horizontal incision at the introitus and a peeling of the posterior vaginal wall cephalad without additional incision of the flap. This exposes the rectocele defect centrally and the medial borders of the levator ani (puborectalis). No tissue is excised. No suturing is done on the rectocele bulge. Sturmdorf describes the plication, "The sutures passed entirely round (not through) the muscle-shanks, encircling them so as to secrure the broadest possible side-to-side surface contact under the vaginal floor." The procedure concludes with a longitudinal closure of the horizontal skin incision. No skin is excised. It is clear that the levator plication sutures are extremely broad and deep. The complete "encirclement" of these muscles and ligation places extreme tension on a large mass of tissue. This will undoubtedly cause ischemia and ischemia will cause significant discomfort in the short term. In the long term, chronic tension on the muscle tissue will predispose to myalgia and traction pain on nerve fibers. The absence of an independent repair of the rectocele bulge creates two problems. First, it places all of the tension of subsequent bowel movements directly onto a single plane of tissue placing additional stress centrally. It would surprise no one that this type of levatorplasty would create pain with sex or any activity that stresses the muscle tissue. Second, it leaves the low-pressure tissue of the rectocele hernia floating, in essence, and free to float cephalad beyond the plication zone and recur later. The most recent of the oft-quoted articles on painful levatorplasty articles was published by Kahn and Stanton in 1997 (BJOG.1997;104:82-86.). They looked retrospectively at 209 British women treated for rectocele using Stanton's mid-century levatorplasty-only method. Painful sex or anatomical difficulty with sex was found in 27 percent, although 18 percent had problems beforehand. Stanton stated that his levatorplasty technique was identical to that of his British colleagues, Lees and Singer (pictured above). The huge needle bites through a large mass of levator muscle tissue indicate an aggressive high-tension approach. The photos also reveal that the rectocele itself is not sutured. Like that of Sturmdorf, this method provokes tension-related issues. In their discussion, Kahn and Stanton opine that dyspareunia is caused by levatorplasty because of "pressure atrophy of the included muscle fibers and subsequent scarring." citing references from the 1920s, but no data (Goff. Surg Gynecol Obstet. 1928;46:855-866). So where does this historical analysis lead us? First, we see that taking huge bites of the levator ani muscle and forcing them together under high tension creates problems. Second, we see that using a single layer of muscle tissue as the only repair for a rectocele creates problems. Third, we see that quoting articles that quote articles doesn't provide data directly and that opinions in the discussion section of published articles aren't exactly the same thing as evidence and might distort the impression of the literature for those who fail to dig a little deeper. I stated that my levatorplasty is not the same as "their" levatorplasty. What's the difference?
It doesn't require huge bites of muscle tissue. It doesn't involve high tension. And it doesn't take place withouit the support of a sturdy rectocele repair underneath to take the tension and stress off the sensitive muscle tissue. Two decades. No problems. No kidding. Would you like to learn more?
Listen to the Expert Panel Discussion from the 2019 ISCG World Congress of Cosmetic Gynecology conducted on January 29, 2019, in Orlando, Florida. Nine world experts with extensive experience in the use of nonsurgical lasers and radiofrequency devices discuss the concerns raised by the FDA regarding the use of these technologies and share their insights and experience. Moderator: Marco A. Pelosi, III, MD. Expert Discussants: Alexander Bader, MD (UK), Rafal Kuzlik, MD, PhD (Poland), Michael Krychman, MD (USA), Michael Goodman, MD (USA), Oscar Aguirre, MD (USA), John Miklos, MD (USA), Red Alinsod, MD (USA), Adrian Gaspar, MD (Argentina), Jorge Gaviria, MD (Venezuela & Spain).
This article was originally published on LinkedIn on August 30, 2018. I just got off the phone from two calls. The first was a surgeon seeking vaginal rejuvenation training and the second was a patient seeking a vaginal rejuvenation procedure. They sought my expertise on two completely different things. The never-been-lucid definition of vaginal rejuvenation is growing in many directions unimagined in years past. On a regular basis, it takes twists and turns as educated proponents, ignorant proponents, and detractors add narrative- and agenda-loaded meanings to this volatile term.
Why is this happening? I see a few major reasons: Foremost is large-scale marketing. Second, is the catalytic effect of social media on a level unknown when the first iteration of vaginal rejuvenation made its debut in the late 1990s. A public whose sole education on the term arises from repetitive marketing to their smartphones and whose knowledge of their bodies appears quite limited has no filter with which to distill whatever the Oprahs and Dr. Ozs of the world feed them via colorful Hollywood-quality vignettes. Their “research” is overwhelmingly a collection of marketing materials dressed up with pseudoscience. It’s time to separate fact from fiction. The Backstory Vaginal childbirth has been has been destroying vaginas since the beginning of time and modern pelvic floor research has been confirming what mothers have known for generations. Focus has been on the vaginal supports, bladder and bowel dysfunctions, and prolapse. Curiously, vaginal laxity is excluded from this conversation in medical circles, in the gynecologic literature and at meetings of large academic gynecologic societies. I invite you to search the term “vaginal laxity” on the websites of ACOG and FIGO, the two largest gynecologic academic societies in the world and that of AUGS, the largest urogynecologic society in the world to witness this void personally. I have yet to find a female patient who states that sex improved after vaginal childbirth. These women have gynecologists who deliver babies every day. Many gynecologists are mothers themselves. They see the vaginal trauma of childbirth day in and day out and experience the aftermath personally. Sadly, I would have trouble swinging a cat in a room full of academic gynecologists without hitting an opponent to the concept that tightening the vagina might improve sex after vaginal childbirth. You can live without treating it. It’s a lifestyle issue they say. True. That was the world pre-1996. But what else can we live without treating – fertility, infertility, unwanted pregnancy, foreskins. All of the latter are essentially lifestyle issues on which the specialty is deeply rooted. The Day Sex Got Better A patient underwent gynecologic anterior and posterior vaginal repairs for medical indications in Beverly Hills, California, in 1996. A few months later she told her surgeon, David Matlock, that her sex life had also improved; she said that it was because her vagina felt tighter. She referred a friend to him for the same operation. She had no medical indications, but she had a lax vagina that she wanted tighter to improve her sex life too. Dr. Matlock acceded to the request. Her sex life improved. Vaginal rejuvenation was born. (ref: conversation with Matlock, 1999) David Matlock, MD, became David Matlock, MD, MBA. In the process, he learned about marketing, intellectual capital, and trademarks. In 1998, he labelled his operation Laser Vaginal RejuvenationTM and added Designer Laser VaginoplastyTM (a labiaplasty procedure despite the name), and the G-shotTM (a dermal filler injection for the G-spot) to his repertoire. Why Laser? Two reasons: Matlock preferred the laser scalpel to the steel scalpel for his anterior and posterior repairs having learned to use the technology in his residency training. Lasers were introduced to the field of gynecology in the early 1970s and were a topic of intense academic and private practice interest and study well into the 1980s and 1990s. Second reason: To this day, “laser” has unparalleled marketing power to patients. A Bodacious Adolescence When you launch Laser Vaginal Rejuvenation in the epicenter of aesthetic culture and entertainment media, it gets noticed. Matlock became a global celebrity. Women added Laser Vaginal Rejuvenation to their Mommy Makeover bucket lists and other surgeons, naturally, wanted in on the action. Matlock saw the potential market and created the Laser Vaginal Rejuvenation Institute of America to train surgeons in his techniques and license his trademarks. He utilized a franchise model and Laser Vaginal Rejuvenation began its widespread growth. Competitors emerged and, unable to use the trademarked terminologies, created their own nicknames for their versions of these procedures. The most common of these was simply vaginal rejuvenation. The End of the Beginning Gynecologic academia had consistently stayed out of the aesthetic/cosmetic arena and periodically reaffirmed this stance in public statements. However, the emergence of social media (Facebook 2004, YouTube 2005, Twitter 2006, iPhone 2007) created a wave of global attention on vaginal rejuvenation on which the academics were forced to offer commentary. In September 2007, the prominent American College of Obstetricians and Gynecologists (ACOG) released ACOG Committee Opinion No. 378: Vaginal "Rejuvenation" and Cosmetic Vaginal Procedures – a document which was parroted by academic societies around the world. A brief five paragraphs and one reference long, this document has been misquoted, misinterpreted and misused widely by people at all levels of intelligence ever since it came out. The opinion attempts to define vaginal rejuvenation, yet opens with the admission that the authors are unclear of the exact nature of the procedures upon which they are opining. It lists Dr. Matlock’s trademarked portfolio procedure-by-procedure sans the word “laser,” yet they neither interviewed Matlock nor observed his work (ref: conversation with Matlock 2007; conversation with ACOG committee members 2008). The second paragraph reiterates the trademarked terminology, questions its safety and effectiveness, and adds that it lacks data. Perhaps, if they had learned that Laser Vaginal Rejuvenation was an alias for gynecologic vaginal repairs with over a century’s worth of robust data, they might have concluded differently. The third paragraph disparages the businesses of franchising, marketing, and paying for education. This is a direct objection to Matlock’s business model, but it didn’t apply to anyone else in the vaginal rejuvenation arena. Hypocritically, most if not all college and postgraduate educational programs require payment to the educators and most if not all academic societies, ACOG included, demand annual fees for the right to use their letters of distinction. The fourth paragraph is best characterized as The Insanity Plea: a woman requesting these procedures needs a long talk to convince her that she’s normal. The lone reference in entire opinion is attached to this paragraph - a study that found that labia minora came in different shapes and sizes in 50 British women. The concluding paragraph complains that women are being misled, that the procedures are not routine, reiterates the lack of data misconception, and out of thin air adds a list of potential complications that may arise from procedures on which the authors already stated they are unclear. The Rise of the Machines For the first decade and a half of it’s existence, vaginal rejuvenation was a surgical procedure for vaginal tightening with a steep barrier to entry - expertise in internal vaginal surgery – skills limited to gynecologists, urogynecologists, and some urologists. Then, the game changed. Beginning in 2009, pioneering gynecologists in Argentina and Italy began developing techniques for nonsurgical laser treatments of the vagina aimed initially at vaginal atrophy. Working in conjunction with the industry’s standard laser platforms, they devised equipment and protocols for fractional carbon dioxide laser ablation based on existing dermatology protocols. Over the next few years, other groups began clinical investigations into the treatment of urinary incontinence and vaginal laxity working with a variety of lasers. This era culminated with the entry of Deka (MonaLisa) and the Alma (FemiLift) CO2 lasers for noninvasive vaginal ablation into the US market in late 2014. From then until now, the market has literally exploded and almost every major laser manufacturer makes a vaginal probe for their platform and radiofrequency technologies have followed suit. The Marketing Paradox How do you market a vaginal laser in the US? This was the challenge for the industry in 2014. Most lasers owners were plastic surgeons, dermatologists and other aesthetic professionals who hadn’t done a pelvic exam since medical school. All of the applications for vaginal lasers to date were purely gynecologic in nature – atrophy, incontinence, and laxity, but most gynecologists weren’t early adopters and wouldn’t buy a laser unless they were sure of a steady market for the service and saw homegrown proof of its efficacy from experts in the field irrespective of the overseas experience. Marketing took a two-pronged approach: For existing aesthetics based laser owners, the theme became nonsurgical vaginal rejuvenation to get a piece of the vaginal laxity market and leave the rest to the gynecologists. For gynecologists, it was marketed first to academically inclined urogynecologists to establish credibility of efficacy. Since many in the gynecologic academic community had been mentally “poisoned” to the term vaginal rejuvenation in 2007 and eschewed any mention of vaginal laxity treatments, vaginal atrophy and urinary incontinence were the exclusive focus. For patients, the terms vaginal health and feminine health were created for direct marketing. Mass Confusion Wins By mid-2015, gynecologists and non-gynecologists alike were marketing laser vaginal rejuvenation, vaginal rejuvenation and nonsurgical vaginal rejuvenation online as synonyms for a variety of surgical and nonsurgical procedures well beyond the original meaning and intent of Matlock’s vaginal repairs. To confound matters further, patients doing online research on incontinence and vaginal atrophy were finding themselves in the offices of non-gynecologists without the benefit of a gynecologic assessment. The confusion persists to this day and continues to worsen as the number of devices and treatments continue to grow. At the present time, vaginal rejuvenation has so many possible meanings that it has no specific meaning. When a woman tells me that she wants vaginal rejuvenation today, I have absolutely no idea what the term means to her and what issues she is seeking to address. It might be a gynecologic issue. It might be an aesthetic issue. It might be surgical. It might be nonsurgical. I also have no idea what her expectations might be as her judgement may have been seriously clouded by whatever “research” she has chosen to believe. Vaginal rejuvenation in 2018 is a conversation starter, an icebreaker. The challenge in the conduct of this conversation is to understand that the average patient is clueless about her body, jaded with the expectations of mass media marketing hype, and completely at the mercy of the physician’s ethical compass. This article was originally published on LinkedIn on August 17, 2018. Recently, the MAUDE database has been cited as a source of “numerous” reports of adverse events associated with the use of transvaginal energy-based devices (tv-EBD). However, those who have cited the MAUDE database have failed to provide specifics regarding the quality, the quantity, and the nature of these reports. Seeking to satisfy my own curiosity, I conducted a search of the MAUDE database for adverse events for every vaginal EBD device and every manufacturer of such devices since they first appeared on the market in late 2014.
The search was conducted online via the FDA’s MAUDE search engine page. The name of each manufacturer, US distributor where relevant, and device was searched individually from 2014 to the present. The number of reports parameter was set to 500, the maximum. Some events had been reported more than once – some by personnel associated with manufacturers, some by physicians, some by patients. I then classified each device by it’s technology: Radiofrequency (RF), Radiofrequency with Active Cooling (RFAC), Carbon Dioxide Laser (CO2), Diode Laser (D) Erbium:Yag Laser (ER), Erbium:YAG + Diode Laser (ERD). These are the results of this search: Alma Lasers: FemiLift (CO2): no adverse events reported BTL Aesthetics: Ultra Femme 360 (RF): no adverse events reported Venus Concept: Fiore (RF): no adverse events reported Inmode: Votiva (RF): no adverse events reported Eufoton: LadyLift (D): no adverse events reported Cutera: Juliet (ER): no adverse events reported Lasering-USA: V-Lase (CO2): no adverse events reported Syneron CO2RE Intima (CO2): no adverse events reported Thermi: Thermiva (RF): 1 report: Gynecologist bruised her patient with device Cynosure: DEKA: MonaLisa Touch (CO2) 3 reports of 1 event dated 3/31/2016 of UTI symptoms after treatment by gynecologist 3 reports of 1 event dated 8/23/2017 of urethral pain after treatment #3 by urologist in patient with hx of chronic urethral pain before tx, positive response with first 2 treatments 2 reports of 8/10/2017 & 9/4/2017 of 1 event: physician burned his own hand b/c assembled laser improperly 1 report 2/11/2016 of pt who had pain after treatment by gynecologist and had medical treatment at local urgent care clinic with vaginal creams and oral pills Sciton: DiVa (ERD): 1 report of two non-physician medical staff who gave each other external burns unsupervised event 2/20/2018 Viveve: Geneveve (RFAC): 2 reports of 1 event: patient experienced multiple symptoms with “trial” handpiece after popping noise Lumenis: FemTouch (CO2): 1 report of patient getting eye infection from eye protection after treatment by gynecologist 1 event of issues cleaning the handpiece The total number of reports in this search was 15. The total number of events was 9. Two of these were non-physicians burning themselves while "playing doctor" with a laser. The total number of events involving patients undergoing treatment was 6. One of these was an eye infection from dirty eye protectors. This leaves 5 relevant events of vaginal issues. Let’s examine these five adverse events involving patients undergoing vaginal treatments with energy based devices. 1. The Thermiva RF bruise event: In 2016, a woman noticed discomfort after treatment by an unspecified operator then went to her gynecologist who diagnosed bruising. Bruising is not a known complication of any low temperature radiofrequency technology used in the vagina, but it is a common occurrence with excess pressure on the vulvovaginal area. I would suspect the latter. The procedure itself involves a gentle massaging motion of a plastic handpiece and does not involve the application of excess pressure. 2. The MonaLisa UTI event: In 2016, a woman noticed urethral burning and discomfort beginning two days after treatment by her gynecologist and persisting for several weeks. Although urinalysis was performed 3 times, no urine culture was performed and no antibiotic therapy was given. The risk of urinary tract infection exists with any manipulation of the vulvovaginal area and is not unique to any procedure or any device. Procedures in the vagina and vulva are categorized as Class II: Clean Contaminated by the CDC with an infection rate of 4 to 10 percent (ref). Up to 20 percent of UTIs have been reported to show a negative urinalysis and culture is the gold standard (ref). One of the 3 reports of this event states that this patient had an active yeast infection that was being treated at the time of her procedure. 3. The MonaLisa urethral pain event: In 2017, a urologist attempted to treat the symptom of chronic urethral pain with CO2 laser fractional ablation. The patient’s symptoms vacillated in response to treatment and overall there was no long term detrimental effect documented. The main issue here was lack of knowledge in the techniques, technology and indications. There is no literature anywhere to support the use of fractional CO2 laser ablation to treat urethral pain and there is no protocol for doing so. This is an example of experimentation. 4. The MonaLisa post-procedure discomfort event: In 2016, A woman experienced discomfort after her procedure and went to an urgent care clinic to have her issue addressed. This report was provided by the manufacturer and was reported because the patient sought and received care from an urgent care clinic. It is not uncommon for patients to seek out care at urgent care clinics. Reasons for doing so may include inadequate pre/post procedure counseling, an inability to contact their treating physician, the suggestion of friend or family member, or convenience. 5. The Geneveve pain event: In 2017, a non-gynecologist treated a woman who had never undergone the procedure before at twice the standard energy dose with a “trial” handpiece that hadn’t been used before. A strange “popping” noise was documented during the procedure, but the procedure was continued. The patient reported pain, sensation issues and urinary incontinence. This event suggests a complete lack of professional judgement and a lack of knowledge of energy based devices on the part of the operator. Although I have no experience with the use of this product, I have 27 years of experience with lasers. Every laser case invokes a strict checklisted laser protocol that involves equipment checking and test firing outside the human body. The latter applies to equipment that is in it’s final form, not a trial device. In the case of a trial device, a trial procedure is done outside the human body on a suitable model where the device can be tested. At that stage, it might be ready for a human trial or not. It is not offered as reasonable treatment to anyone as this is purely experimentation. Arbitrarily doubling the energy dose in a treatment-naïve patient is without precedent in any energy-based therapeutic intervention that I am aware of and cannot be justified. Ignoring an inexplicable noise during operation of the device is unfathomable. This unfortunate event can be deemed a compounding of errors stemming from extremely poor clinical judgement. This analysis of the MAUDE database brings several issues to light. First, is the need to distinguish the number of events from the number of reports of singular events. Every year, my birthday is reported “numerous” times by my Facebook friends. This happy birthday effect does not elevate the magnitude of this singular event. Second, is the need to educate “rookies” to EBD in the technologies they are using, to the indications of the treatments they are providing, and to the counseling and postprocedural support that their patients may require. All of these five adverse events can be classified as human factor errors. My colleagues from other specialties suggest that I am inciting a turf war. To the contrary, I am offering simple advice for staying out of trouble. So many “skin experts” that I know offer elaborate skin imaging and mapping technologies prior to facial EBD treatments, yet offer no vaginal assessment whatsoever prior to firing a laser or other EBD in the vaginal canal blindly. Third, is the need to establish a collective database of experience with the devices. The MAUDE system does not and cannot track the number of procedures performed. It can only offer a glimpse into the issues of reported events and it is severely limited at that. When estimating the unknown frequency of true adverse events, pundits against EBD will exaggerate the numerator and dwell on the few available sad vignettes while those who favor EBD will stress that there is no denominator, but that it’s probably large. This article was originally published on LinkedIn on August 5, 2018. One week ago, tomorrow, the FDA issued a Safety Communication slamming the use of energy-based devices for the indications of "vaginal rejuvenation" - "an ill-defined term" - "sometimes used to describe non-surgical procedures intended to treat vaginal symptoms and/or conditions including, but not limited to:
Vaginal laxity Vaginal atrophy, dryness, or itching Pain during sexual intercourse Pain during urination Decreased sexual sensation" The document stated that there are two problems: 1. "To date, we have not cleared or approved for marketing any energy-based devices to treat these symptoms or conditions, or any symptoms related to menopause, urinary incontinence, or sexual function." 2. "The treatment of these symptoms or conditions by applying energy-based therapies to the vagina may lead to serious adverse events, including vaginal burns, scarring, pain during sexual intercourse, and recurring/chronic pain." The document lists two references:
The first of these references was written in 2007, almost a decade before these energy-based devices ever existed. It obviously makes no mention of any energy-based device nor any mention of the treatment of any of the vaginal symptoms listed in the current FDA document. The second reference, published in mid-2016, was essentially a clarification of the FDA approval language for fractional CO2 lasers in gynecology drafted by the American College of Obstetricians and Gynecologists. This document stated that the FDA had not approved these lasers for the indication of vulvovaginal atrophy (VVA) and that preliminary observational data had shown some potential benefits with the use of this technology in treating patients with VVA. It made no mention of any adverse events. This document listed 6 references, 3 of which were short term clinical studies of this technology for VVA, and none of which made mention of any of the adverse events listed in the current FDA document. To summarize, the FDA has proof that energy-based devices are being marketed for indications that were not part of the FDA approval, and the FDA has no proof that the use of these energy-based devices for these indications is causing any of the serious adverse events listed in their Safety Communication. I have been involved as both a user and a consultant to the industry on these devices since their FDA approval. I have extensive training, education, and experience in the treatment of vaginal atrophy, urinary incontinence, vaginal laxity, and lasers. I am consulted when physicians have problems with these technologies and the problems have never been related to adverse events. I have witnessed the explosion of marketing for these indications by the industry and I am very well aware of the paucity of data to support the use of these technologies for these indications. However, in my experience, these technologies work well in carefully selected patients. I haven't seen the serious adverse events listed in the Safety Communication. I have conducted and attended professional conferences on the topic of these technologies, constantly review the literature, and constantly consult with both experts and neophytes in these technologies and haven't heard of physicians experiencing the serious adverse events listed in the Safety Communication. So from where did this list of adverse events originate? I can only speculate that this list has been carried over from other applications of CO2 laser technology that did not involve fractional ablation or the relatively low energy settings used in the vagina. These machines have the capability to do more than fractional laser ablation of the vagina. They are designed for multiple uses all over the body. Certainly, if misused intentionally, they hold the capability to burn tissue severely. However, and despite the fact that out-of-control marketing has put these devices into the hands of physicians with little or no training in the indications or the technologies in question, there is no evidence that I am aware of that we are in the midst of a laser vagina trauma epidemic. One would expect a perfect storm of morbidity under such conditions. To the contrary, the current lack of adverse reports would suggest that these devices used as recommended are idiot-proof. Would the FDA withhold proof of serious adverse events in a Safety Communication? Highly unlikely. There would be no motive. Especially, at the present time, when the FDA is proudly launching it's Medical Device Safety Action Plan. If anything, such proof would only add emphasis to their statement. A relevant example, would be a recent Safety Communication against injectable silicone published 9 months ago where the references offer ample proof of serious adverse events associated with that product. In my opinion, the main risk of these technologies to patients, is the lack of an expected treatment effect. Expectations should be based on both personal and published experience, patient counseling, and intimate knowledge of the conditions being treated and of the techniques and technologies being considered. This is the essence of solid clinical judgement. In their own words, "The FDA does not have the authority to: Regulate a physician's or nurse's practice. FDA does not tell providers what to do when running their business or what they can or cannot tell their patients. Make recommendations for individual doctors, clinics, or home care agencies. Conduct or provide a rating system on any regulated medical devices." However, it is their duty to make physicians and the public "aware" and "understand" issues related to product safety and effectiveness for the uses for which they are approved. An overzealous allusion to adverse effects unsubstantiated by data is out of place and does not a perfect storm make when all that can be seen are clear skies.
This lecture was given as the finale to the 2018 ISCG World Congress in Las Vegas. It summarizes trends in the specialty and comments on issues and criticisms.
This is a lecture delivered to the New Jersey Obstetrical and Gynecological Society at their 66th Annual Meeting. It is a complete introduction to the field of cosmetic gynecology and covers the major issues and controversies. I wrote a review article on cosmetic vaginal surgery for the short-lived internet journal US Obstetrics & Gynecology a while back. With their website gone, the links to this fine manuscript have evaporated into the abyss of The Cloud. Back from the ashes, here it is slightly updated: AbstractA variety of procedures are available for the cosmetic enhancement of the female genitalia. Despite controversy, they continue to grow in popularity. Familiarity with the terminology and spectrum of the aesthetic options described herein permits a realistic assessment of the ways in which the female patient’s concerns may be addressed. There are important aspects of patient evaluation and counseling unique to cosmetic surgery that must be learned by those contemplating the delivery of these services. IntroductionCosmetic vaginal surgery encompasses aesthetic procedures directed at the appearance of the vulvar structures and tightening procedures directed at the reduction of vaginal caliber. The most commonly treated areas are the external vulvar structures. These include the mons pubis, the labia majora and the labia minora which includes the clitoral prepuce. The perineum and the lower third of the posterior vaginal wall are the areas typically operated in vaginal tightening procedures. The anterior vaginal wall does not play a role in vaginal tightening. Hymenoplasty is performed when requested for cultural reasons. Like cosmetic procedures of the face, the breasts and the body, vaginal procedures focus on the elective alteration of normal structures. They are not treatments for medical conditions and offer no health benefits. Unlike these other established cosmetic procedures, the first public wave of cosmetic vaginal surgery emerged from the work of corporate-style entities which branded their procedures and treated their technical knowledge as private intellectual property. Over the past decade, cosmetic vaginal surgery has reached public awareness on par with other cosmetic procedures and a growing number of gynecologists, cosmetic surgeons and plastic surgeons are offering these services to their patients. The reasons behind the increased demand for this type of surgery has been postulated by many groups, but not established by any type of scientific analysis. Many have used this information vacuum as an opportunity to advance or regurgitate chronic agendas against cosmetic surgery in general. Our impression as surgeons performing this type of surgery as well as a wide range of established cosmetic procedures is that the rapid growth of these procedures is due to three factors. First, is timing. The first half of the past decade witnessed the greatest surge in cosmetic medical and surgical volume in history. Yearly statistics monitoring the cosmetic activities of ENT, dermatology and plastic surgery specialists demonstrated a six-fold increase in total cosmetic procedures between 1997 and 2006 (ASAPS, 2007). Cosmetic vaginal surgery emerged during this era and became a component of the intense media coverage which brought cosmetic surgery onto television shows and other media. Second, is the global cultural shift into social media communications as the internet and advanced mobile devices created a level of awareness and information access unprecedented in human history. It is not only possible, but simple, for anyone anywhere to access media on any topic at any time without censorship. Access to services is relatively unimpeded. Third, depilation of the mons pubis has become as popular as that of the legs and axillae in the United States. Once depilated, these areas have now become targets of decoration with tattoos, piercings and surgical modification. A background in gynecology is ideal for evaluating the prospective cosmetic vaginal surgery patient because gynecologic disease or dysfunction may be aggravated if a procedure is performed at the wrong time (e.g. vaginal tightening in a woman who plans on delivering vaginally in the near future or in a woman who has significant pelvic floor defects). However, the evaluation of the cosmetic patient also warrants attention to psycho-social factors which might lead to unrealistic or unachievable expectations such as the presence of body dysmorphic disorder, immaturity, a perfectionist mentality, a cosmetic surgery addiction, a belief that surgery will cure interpersonal problems or a desire to have surgery for the benefit of a partner. These issues are common screening criteria for all cosmetic surgical procedures, but gynecologists who enter this field with a broad knowledge of gynecology, but little familiarity with the cosmetic patient may find these issues to be a new dimension previously unexplored. The Cosmetic Gynecologic AssessmentUnlike the medical patient who seeks relief from disease, deformity or dysfunction, the cosmetic patient must meet be completely healthy in order to be an appropriate candidate for a procedure which offers no health benefit. The well-chosen patient fall into either category ASA I or ASA II of the American Society of Anesthesiologists Physical Status Classification System, but those with specific diseases with a known predisposition to poor healing or increased surgical morbidity such as diabetes or hypertension are best avoided. Hospitalization costs associated with cosmetic procedures, planned or unplanned, are not covered by conventional healthcare insurance. Following the initial conversation regarding the cosmetic request and the requisite psycho-social analysis, the physical examination is conducted. For cosmetic requests involving the vulvar structures or mons pubis, the physical examination is best conducted with the patient standing before a full-length mirror because this is typically the position in which they wish the appearance to be altered. The standard gynecologic dorsal lithotomy position is then assumed to better examine the full extent of the vulvar structures and to conduct a full gynecologic examination include an assessment of any infection which may interfere with the surgical procedure. For vaginal tightening operations there is no need for the standing examination unless there is suspicion of pelvic organ prolapse. However, there is a need to assess the existing width of the levator hiatus and the quality of the puborectalis muscle tone since this will be the focus of these procedures. A common practice is to measure the hiatus in fingerbreadths with the muscles at rest and with the muscles contracted then convert this data to centimeters. Peri-Operative CareAnesthesia requirements for cosmetic vaginal surgery are no different than those for any other vaginal procedure and can be either general, epidural, spinal or intravenous sedation with local block. Prophylactic antibiotics are routinely employed immediately before surgery. Patients are positioned in dorsal lithotomy with the legs supported in boot-type stirrups with mild flexion of the knee. Intermittent pneumatic compression stockings are routinely employed. Indwelling bladder catheterization is employed during most operations. Bladder catheterization is maintained postoperatively for 24 hours in cases where periurethral swelling is anticipated and in cases in which vaginal packing is placed. The Mons PubisThree common cosmetic treatments are available for the mons pubis. The first of these is simple depilation of the pubic hair. The techniques and technologies are the same as those used elsewhere on the body and include laser or intense pulsed light (IPL) treatments administered in a series of sessions over an interval of several months. Multiple sessions are necessary because hair follicles are sensitive to therapy at only certain points in their growth cycle and at any given time, only about 25% of these follicles are in the requisite phase. Modern depilation technologies do not result in total depilation, but greatly reduce the density of hair follicles and the frequency with which any additional depilation maneuvers (shaving, waxing) are needed. The technologies are limited by the degree of melanin and skin pigmentation present and are not advisable for the darkest skin types. Liposuction of the mons pubis is a common procedure for the treatment of excess adiposity and is usually performed in conjuction with abdominal liposuction. The treatment tapers off into the anterior margin of the labia majora. Tumescent local anesthesia – a solution of saline, lidocaine, epinephrine and sodium bicarbonate – is the most common type of anesthetic used for this procedure. Mild postoperative swelling and slight temporary bruising extending to the labia majora are common in the first week after surgery. Mons pubis liposuction is also performed as an adjunct to abdominoplasty when the inferior edge of the incision line is significantly thicker than superior flap. The mons pubis lift is a derivative of abdominoplasty techniques and targets significant laxity in the mons pubis region and sagging of the labia majora as viewed in the standing position. The procedure entails careful controlling of the central tension vectors when planning the resection pattern at the time of abdominoplasty. Whether the procedure is isolated or part of a larger abdominoplasty, excess tension at the lateral angles of the pubic triangle and curving the center of the scar cephalad are two aspects of the surgery which need to be avoided to generate an optimal cosmetic result. These goals are best accomplished with a high lateral tension-style excision pattern. The pubic lift integrates well with mons pubis liposuction. Mons pubis lift with abdominoplasty. A. Surgical markings demonstrate incision line (red) and bikini lines (black). B. Traction is applied to mons pubis after preliminary liposuction has been completed and vectors are studied for adequacy. C. Vectors are reassessed at time of flap closure. D. Appearance at six months post-surgery. The Clitoral RegionLoose, redundant folds of skin lateral to the clitoris are the target of cosmetic excision in this region. This tissue is contiguous with the skin of the clitoral hood (prepuce), but does not function to protect the glans clitoridis. These skin folds may be as large as the main clitoral body and precise dissection in a direction and depth that avoids the path of the clitoral sensory nerves is essential to maintain full sensation. Maintenance of symmetry is another essential aspect of the surgery as the resection of too much skin may pull the clitoral alignment away from the midline. Since this is cosmetic surgery, camouflage of the suture lines is desirable. To this end, incisions across the dorsum of the prepuce along the clitoral shaft should be avoided because they will be visible when the patient is viewed in the standing position. Maintaining incision lines parallel to or within the natural skin folds produces an effective camouflage and is very difficult to detect. When planning surgery of this type in combination with an abdominoplasty or a mons pubis lift, the lift is done first because it frequently produces a tightening of the prepuce in the vertical axis when the mons pubis is placed on cephalad traction. The Labia MinoraReduction labiaplasty of the labia minora is one of the most commonly requested cosmetic vaginal surgery procedures. Common presenting complaints include dissatisfaction with elongated, asymmetric or hyperpigmented labial tissue. Less frequently, patients will request repair of chronic torn labial tissue years subsequent to vaginal delivery. A thorough examination of the labia minora, from a cosmetic perspective, necessitates splaying them laterally onto the labia majora to determine the degrees of hypertrophy, hyperpigmentation and asymmetry which may be present. Proposed excision lines are marked and demonstrated to the patient with a hand mirror. Anteriorly, the planned excision lines may end inferior to, at or beyond the clitoral frenulum. Posteriorly, the excision line may extend toward the fourchette in the midline. When combined reduction labialplasty and vaginal tightening procedures are planned, vaginal tightening is performed first because it involves the resection of the existing fourchette. Laterally, resection should never extend beyond the natural crease between the labium minus and the labium majus because the tension which results may produce gaping of the vaginal introitus and expose the urethra. Suture lines are dressed with topical tissue sealants at the conclusion of surgery and patients are instructed to avoid tight clothing for the first two weeks, to avoid inserting anything in the vagina for six weeks, and to avoid prolonged sitting on the suture lines for six weeks. Local edema and bruising are common in the first two weeks following these operations. Left labia minoraplasty for the relief of sports-related traction pain at the time of a bilateral procedure. Inset illustrates the natural crease between labium minus and labium majus which must be preserved to prevent gaping of the vaginal introitus. Larger photo demonstrates appearance labial base. The left clitoral crus and bulbocavernosus muscle are clearly demonstrated. Right sided reconstructive labia minoraplasty for chronic second-degree tear with associated traction dyspareunia. A. Arrow indicates defect which involves the insertion of the clitoral hood to the labium minus dorsum. B. With the corners of the defect on traction, the scar tissue has been excised in preparation for repair. C. Appearance immediately following a three-layered reconstruction. The Labia MajoraLoose sagging skin, loss of volume, varicosities and unwanted hair are the common complaints of women seeking alteration of labia majora appearance. Redundant skin is best managed by longitudinal ellipsoid resections of skin and subcutaneous fat. Aggressive dissection along the course of the sensory nerve supply to the labia and clitoris should be avoided. Absolute hemostasis is critical in this highly vascular and very elastic tissue as large hematomas can easily develop. Volume loss is addressed by autologous fat transfer into the subcutaneous fat layer. Fat is harvested from any convenient site using conventional liposuction techniques and typically requires less than 50cc for a bilateral augmentation. Fat injections are performed with specialized blunt-tipped needles to avoid the risk of cannulating blood vessels inadvertently. As the fat is injected into the area, it is molded into the desired shape by pressure and massage. Some loss of the implanted fat volume is expected and the need for multiple fat transfer sessions is anticipated. Varicose veins of the vulvar region respond to sclerotherapy in much the same manner as those of the lower extremity. Not infrequently, these varicosities are a source of pelvic pain and a gynecologic workup for pain should rule out other etiologies prior to treatment. Common sclerosing agents such as sodium tetradecyl sulfate are used and administered via small-guage needles attached to tuberculin syringes. The veins are targeted in the standing position and injected in the supine position. The technique is identical to sclerotherapy of the leg varicosities working from proximal to distal veins. A pelvic compression garment is worn for the first week post-injection. Left sided reconstructive labia majoraplasty for a non-communicating hydrocele. A. The extent of the distortion is demonstrated. B. The skin resection margins were marked in the standing position and are demonstrated in dorsal lithotomy. C. Mobilization of the cyst extended along the canal of Nuck and ended at the level of the pubic symphysis. D. Appearance immediately after layered cosmetic reconstruction and Dermabond dressing. Patient presented for augmentation labia majoraplasty with fat injections and treatment of isolated vaginal laxity. A. Attenuation of the perineal body is demonstrated and marked for resection. B. Fat was harvested from the inner thighs using syringe liposuction. C. Following the completion of a modified posterior colpoperineorrhapy, approximately 20 cc of purified fat was injected into each labium majus using a blunt-tipped fat transfer cannula inserted through a needle track incision. D. Immediate post-surgical appearance. Vaginal Tightening (Vaginal Rejuvenation)Procedures for tightening the vaginal caliber are derivations and variations of posterior colporrhaphies and perineorrhaphies. Unlike therapeutic operations targeting significant rectoceles, the focus of these operations is less on the repair of the endopelvic fascia than it is on achieving a reduction of the levator hiatus. The fascial repairs remain important ot the durability of the results, but they are not the technical endpoint for the surgeon. In the absence of advanced degrees of pelvic organ prolapse, mild to moderate degrees of vaginal laxity can be corrected quite adequately by targeting the lower third of the posterior vaginal wall and the perineal body for plication. We do not recommend anterior colporrhaphies for vaginal tightening because they do not add significant tightening at the sites most commonly noted by patients to be loose. Also, gauging the degree of tightening can be tricky in inexperienced hands and those considering offering these surgeries to their patients are well advised to seek specific training in these operations from experts. ConclusionA variety of procedures are available for the cosmetic enhancement of the female genitalia. Despite controversy, they continue to grow in popularity. Familiarity with the terminology and spectrum of the aesthetic options described herein permits a realistic assessment of the ways in which the female patient’s concerns may be addressed. There are important aspects of patient evaluation and counseling unique to cosmetic surgery that must be learned by those contemplating the delivery of these services. References1. Pelosi MA III, Pelosi MA II. Breast augmentation. Obstet Gynecol Clin N Am 2010;37:533-46.
2. Pelosi MA III, Pelosi MA II. Liposuction. Obstet Gynecol Clin N Am 2010;37:507-19. 3. Matlock DL. Letter: Cosmetic therapies in obstetrics and gynecology: putting a toe in the water. Obstet Gynecol 2008;112:703. 4. Pardo J, Sola VD, Ricci PA, Guiloff EF, Freundlich OK. Colpoperineoplasty in women with a sensation of a wide vagina. Acta Obstet Gynecol Scand 2006;85:1125-7. 5. Miklos JR, Moore RD. Labiaplasty of the labia minora: patient indications for pursuing surgery. J Sex Med 2008;5:1492-5. 6. Laube DE. In reply to: Indman PD. Letter to the editor: Cosmetic therapies in obstetrics and gynecology practice: putting a toe in water. Obstet Gynecol 2008; 112: 704-5. 7. DeSousa A. Concerns about cosmetic surgery. Ind J Med Ethics 2007 Vol. 4, No. 4: 171-3. 8. Cosmetic Surgery National Data Bank. 2007 Statistics. New York (NY): American Society for Aesthetic Plastic Surgery; 2009. I wanted to share a small sample from an upcoming chapter entitled Cosmetogynecology Note: I took a few liberties with the official version of my work as it will appear in the published version to provide you, the blog reader, with some behind-the-scenes perspectives and anecdotal observations that I usually omit for both brevity and lack of published references from more "learned" discussions. Also, I have included images that exceed those of the to-be-published work because there are no restrictions on quantity here. Bon apetit!  Dr Shirith Sheth Dr Shirith Sheth Shirith S. Sheth, FRCOG Ad Eundem, FACOG (Hon), is an exquisitely skilled, renowned and celebrated gynecologic surgeon from Mumbai, India. He is also a good friend to my surgical team and an individual whom we see much too infrequently. Over a decade ago, we contributed chapters to his excellent book entitled Vaginal Hysterectomy which he co-edited with Dr. John Studd. Several months ago, Dr. Sheth decided that his masterpiece was due for an overhaul and asked if we would be so kind as to update our chapters. He also asked if there was "anything new" that might add to the appeal of the book. Ergo, a chapter on cosmetic gynecology, to be released early next year. We hope you'll like it. LABIA MINORAThe labia minora display a wide range of shapes, sizes, pigmentation and frequent asymmetry. Controlled precise resections are employed to reshape the labia and the skin around the clitoral hood. Some requests are purely cosmetic, others address pain or irritation associated with certain activities such as sex, horseback riding and other sports. Symmetry, balance and comfort are the most common reasons why women request cosmetic alterations of the labia minora. In some instances, treatment is unilateral. Two of these cases presented with complaints of traction pain with various activities. The other two simply disliked the appearance. Can you match the symptoms with the images? - of course not! Myriad techniques for labia minoraplasty abound. They can be categorized into three general groups: (1) linear excisions parallel to the labial edge, (2) wedge excisions perpendicular to the labial edge, and (3) partial-thickness excisions. All of these approaches have been described with variations on the shape and extent of the basic concepts. Linear Labia MinoraplastyModern linear excisions are radically evolved from the simple amputations of antiquity which were originally preferred for their speed in the pre-anesthetic era. The refined cosmetic approach involves a layer-by-layer contoured dissection with hemostatic adjuncts such as vasoconstrictor injections and frequently electrosurgical, radiofrequency or laser coagulation. Linear excisions offer the ability to remove and reshape the entire length and profile of the labial edge. They also allow for precise tension adjustments and typically yield a low-tension suture line and do not generate posterior traction on the clitoral frenulum. If there is a marked color discrepancy between lateral and medial labial skin, this style of labiaplasty may leave an unnatural color transition line along the new labial edge if an aggressive excision is performed. In a full-length excision, 3 to 4 small arterioles will be encountered and require surgical control. Wedge Labia MinoraplastyMarc Laufer (pictured), and William Galvin, pediatric gynecologists at Children's Hospital/ Brigham & Women's Hospital, Boston, Massachussetts, published a 2-case report introducing the wedge labiaplasty technique in 1995 (Adolescent and Pediatric Gynecology 1995;8:39-41). Three years later, Gary Alter, a plastic surgeon from Los Angeles, published a 4-case series introducing the wedge labiaplasty technique. (Annals of Plastic Surgery 1998;40:287-90). In fairness to Alter, I was unable to find Laufer's paper in any medical database using 2013 search technology with a copy of Laufer's paper right in front of me. So how did I find Laufer's obscure paper? He self-referenced it in a 2011 article on pediatric labiaplasty. Wedge excisions offer the ability to preserve the natural labial edge, but cannot reshape the full length of the labial margin. The approach was originally conceived in an effort to reduce scarring and discomfort associated with improperly performed linear excisions (Laufer 1995; Alter 1998). They are a reasonable option when the tissue targeted for excision is limited to a narrow segment of the labium. In a typical wedge excision, a single arteriole is encountered. Wedge excisions near the clitoris have a tendency to draw the frenulum and clitoral hood posteriorly. Attempts to extend the aesthetic reach of this style of labiaplasty by either wider wedging or creative flapping are met by an unacceptably high rate of either incisional dehiscence or tissue necrosis. Partial-Thickness Labia MinoraplastyPartial-thickness skin-only excisions of the labia minora have been proposed with the goal of preserving the labial edge. Two techniques have been described. One of these entails triangular epithelium-only excisions parallel to the long axis of the labium on the medial and again on the lateral aspects. The stroma and vascular supply are not disturbed (Choi et als.). A second approach consists of the resection of a skin-only wedge from the central portion of the labium and consistently leaves a thickened appearance. Clitoral HoodEssentially a component of the labia minora aesthetic unit, the clitoral hood (prepuce) varies greatly in anatomy. Frequently, one finds reduplication of the labia minora extending laterally or bilaterally parallel to the shaft of the clitoris. In other instances, the clitoral hood itself displays loose, redundant folds. Targeted, superficial direct excision of this redundant tissue is individualized. The best cosmetic results are achieved by maintaining suture lines parallel to the clitoral shaft. A cosmetic error, frequently seen with improperly designed linear excisions, is the abrupt termination of the labiaplasty scar at the clitoral hood, leaving a loose redundant mass of periclitoral skin. These require revisionary surgery to essentially complete the procedure. That's it!
If you want more, you'll have to buy the book or see me in person. This was the topic of a recent lecture I gave at the American Society of Cosmetic Breast Surgery annual meeting in Newport Beach, California. The slide show sans narration is available here. It is also the topic of an upcoming chapter in a book edited by Melvin Shiffman. IntroductionBreast augmentation with injections of autologous fat harvested by liposuction was first described in the mid 1980s (2). Early enthusiasm worldwide was soon tempered by concern, albeit speculative, that such transplants would confound or delay the radiologic diagnosis of breast cancer (3). Ongoing critical analysis over recent years has demonstrated, however, that these concerns do not appear to be heightened in comparison to other cosmetic breast procedures and these findings have stimulated a renewed interest in this type of breast augmentation (4,5). To date, this procedure appears best-suited for small-volume augmentation and for cosmetic tissue remodeling around existing synthetic breast implants and sometimes requires multiple treatment sessions to achieve a desirable lasting result (Figure 1). The terms lipofilling, lipomodeling, and lipoinjection are synonyms used to describe autologous fat transfer. Structural fat grafting refers to a specific technique of autologous fat transfer (4). IndicationsThere are two indications for breast augmentation: (1) a cosmetic desire to have larger breasts, and (2) reconstruction of congenital or acquired breast deformity or absence. The best candidates for breast augmentation by any modality are nonobese women displaying relatively symmetrical breasts, a symmetrical frame and lacking breast ptosis. Ptosis is evaluated with the patient standing and is defined as descent of the center of the nipple-areola complex (NAC) below the level of the inframammary fold (IMF). Grading systems are described elsewhere (6). The best candidates for cosmetic breast augmentation by autologous fat transfer are those seeking a modest increase in size, who (1) have adequate fat deposits for harvest by liposuction, (2) understand that an unpredictable proportion of the transplanted fat and associated volume, will resorb during the healing phase, (3) are aware that multiple sessions may be required to achieve a suitable size increase, and (4) are aware that saline or silicone implants are options that deliver predictable size augmentation and they reject those options. A subgroup of patients requesting breast augmentation with autologous fat are primarily interested in liposuction body contouring. Their motivations for breast augmentation lie more in the financial convenience of combining the body contouring procedure with autologous fat transfer and are less interested in attaining a specific increase in breast size. Nonetheless, they should always be counseled regarding the limitations of the breast augmentation with autologous fat and of the other common breast augmentation options. The correction of contour irregularities around existing saline or silicone breast implants is a less common, but effective application of autologous fat transfer to the breast. It is prudent in such cases to be fully prepared to perform an implant exchange at surgery in the event of accidental implant perforation. Rippling and upper pole volume deficiencies respond well to fat transplantation. Capsular contracture has been reported to improve after fat grafting around the constricted capsule (4). Screening & EvaluationGeneral screening criteria for liposuction, then specific criteria for breast surgery are employed. Since breast augmentation by autologous fat transfer typically generates only a modest increase in breast volume, it essential to determine that the patient is not seeking a larger increase in breast volume. Otherwise, the patient will be dissatisfied with the result and with the surgeon for not offering an alternative better suited to her desires. The ideal cosmetic breast patient has no breast symptomatology, pathology, or risk factors for breast disease. Breast specific screening begins with a thorough history and family history followed by a complete physical examination of the breasts with attention to any masses or lymphadenopathy. A history of breast cancer treated by conservative resection is an absolute contraindication to the procedure. Mammography is performed on patients meeting either medical diagnostic or routine screening criteria. Some surgeons prefer to screen all cosmetic breast patients with mammography prior to surgery because of concern that postsurgical changes may obscure subsequent breast cancer screening. All patients are counseled that cosmetic breast surgery may produce calcifications, cysts or palpable lumps that may require diagnostic imaging and interventions including biopsy and can never be assumed to be benign. Medications, supplements, herbs and other substances with the capacity to impair coagulation should be discontinued in advance of surgery. Substances which interact negatively with anesthetic agents and perioperative medications should also be withheld. If they cannot be discontinued or substituted, the surgical plan will need to be modified, delayed or withheld. Cigarette smoking is not a contraindication to liposuction nor to autologous fat transfer, but smokers typically display an atrophic dermis and less skin elasticity which both increase the likelihood of postoperative skin wrinkling. They also demonstrate greater resorption of transplanted fat. Photography of the breasts prior to surgery, before and after marking their measurements, completes the preoperative process. Written release forms specific to photography are mandatory. A routine that includes frontal, oblique and lateral views with arms both at rest and elevated provides an accurate record of asymmetries and of any preexisting scars or contour deformities. External Tissue ExpandersBreast augmentation with external tissue expanders was introduced in 1999 (7). The method, currently known as the Brava system, utilizes a pair of self-sealing rigid polyurethane domes which are applied directly over the breasts to create a negative pressure which causes tissue distraction which, in turn, stimulates tissue growth. Although the technology is effective, it has not gained popularity because it requires a minimum of ten hours of continuous daily use for a minimum of ten weeks to produce results and the results, under the best of circumstances, are typically less than a one-cup size augmentation. More recently, however, the Brava device has been utilized as a means of expanding the superficial planes of the breast in preparation for autologous fat transfer allowing for more fat to be injected under less pressure. The protocol under study involved 4 weeks of pre-operative Brava use for 10 hours daily followed by postoperative use as a shape-supporting stent for the first 7 days (8). Adipose-Derived Stem & Stromal Cells (ADSCs)Multipotent stem cells present in adipose secrete potent growth factors which have been shown to enhance tissue survival in certain settings (9). These findings have stimulated novel techniques of autologous fat transfer that enrich the concentration of stem cells in the harvested fat in preparation for injection (10). Theoretical benefits of adding ADSCs to the harvested fat include: (1) ADSC differentiation into adipocytes, (2) ADSC differentiation into endothelial cells with subsequent increase in blood supply, (3) ADSC release of angiogenic growth factors, (4) ADSC-mediated protection from graft ischemia, and (5) accelerated wound healing (9). Theoretical concerns that ADSC-enriched grafted fat might stimulate the development of breast cancer in vivo have not been supported by clinical findings to date (11). Presently, the use of ADSC-enriched fat in breast augmentation remains in its infancy and there is no clinical data to suggest that it outperforms non-enriched fat in vivo. Platelet-Rich Plasma (PRP)Recent commercial marketing of platelet-rich plasma (PRP) as an aesthetic filler and as an agent with the potential to enhance “handling characteristics of autograft” (12) has prompted the development of multiple techniques and applications of PRP-enriched autologous fat. PRP contains growth factors active in the initiation of wound healing which, in theory, might prove beneficial to the survival of grafted fat. However, the only data currently available relates to in vitro studies (13). A recent small retrospective review of 42 women augmented with autologous fat, 25 of whom received PRP-enriched fat, demonstrated no effect of PRP enrichment on aesthetic outcomes or rates of liponecrosis (14). In our experience, we find that the addition of PRP to centrifuged fat in a 1:10 ratio thickens the consistency of the fat and helps in maintaining the contours of the recipient site in the immediate postoperative period whether it be breast or other sites. Surgical MarkingsThe breasts are marked with the patient standing and the arms down. The margins of the breast mound are marked circumferentially. The breast is divided into quadrants with radial lines drawn from the areolar edge to the margins of the breast mound at the 12:00, 3:00, 6:00, and 9:00 positions. Areas within these quadrants requiring extra volume are then marked and photographed. Operative TechniqueBreast augmentation by autologous fat transfer and fat harvesting by liposuction is typically performed under tumescent local anesthesia (TLA) with or without supplementary intravenous sedation; the latter is employed to calm unusually anxious patients and is conducted by an anesthesiologist. General anesthesia is unnecessary because TLA results in total anesthesia of the targeted tissues. However, techniques which also target fat injection into the pectoralis major muscle utilize general anesthesia (4). Broad spectrum prophylactic antibiotics targeting skin flora are administered intravenously immediately prior to surgery and the patient is positioned in the supine position with the arms away from body. Continuous noninvasive monitoring of blood pressure, pulse oximetry and 3- or 5-lead EKG are instituted. The skin is scrubbed with chlorhexidene or betadine and latex free drapes are applied. The procedure begins with TLA infiltration of the harvest areas and of the breasts. The harvest sites are infiltrated to a tumescent level of tightness by standard techniques described elsewhere (15). TLA is administered via infusion pump and a long spinal needle (18G x 6”, Quincke tip). TLA concentrations per liter of normal saline are as follows: lidocaine 750mg, epinephrine 1mg, sodium bicarbonate 10mEq (8.4% x 10ml). The total lidocaine dose should not be allowed to exceed 50mg/kilogram of body weight. We prefer sharp spinal needles over reusable blunt-tipped infiltration cannulas because (1) they pass through the dense breast connective tissue with far less resistance and tissue drag which results in smoother and more precise guidance by the surgeon, and (2) by the nature of their design, spinal needles deliver the anesthetic fluid wave ahead of the sharp instrument tip thereby minimizing any painful needle tip sensation by the patient. TLA infiltration of the breast in preparation for autologous fat transfer is distinct: A low-volume infiltration of TLA is administered superficially over the entire breast mound approximately 1-cm in thickness. A deeper infiltration is not carried out because the autologous fat is injected superficially. A larger volume infiltration will distort the tissues and impede the accuracy of the augmentation. TLA infiltration begins in the center of the breast mound at the 12:00, 3:00, 6:00, and 9:00 positions at the areolar margin. The skin at these sites is anesthetized with a small wheal of TLA delivered through a small needle (30G) prior to inserting the spinal needle. The spinal needle is then advanced parallel to the skin changing direction in a fan pattern at a low infusion rate. Once the breasts and the harvest sites have been anesthetized adequately, liposuction fat harvesting is carried out using standard technique (15). Cannulas of 3-mm diameter or narrower are preferred because they deliver small fat parcels which are easy to inject through narrow fat transfer cannulas and produce a smoother fill. Fat is collected in either a syringe or in a sterile large-volume glass canister connected to the working cannula via sterile tubing and to the liposuction aspirator pump via a second sterile tubing line. It is important to keep the aspirator suction pressure low (300-330mm Hg) during harvesting to minimize barotrauma to the adipocytes. Centrifugation of the aspirated fat helps to remove blood and excess fluid in order to achieve a more accurate fill of the breast. Centrifugation is carried out in 10-cc syringes at 3,000 rpm for three minutes; oils and fluids are decanted from the top and bottom of the syringe, respectively Centrifugation typically results in the reduction of the apparent volume of fat in the lipoaspirate by one half. Thus, we target a fat volume collection endpoint of twice the desired fill volume. Since we usually inject a maximum of 200ml of fat per breast, we seek to collect 400ml of fat per breast in the lipoaspirate whenever feasible. Naturally, in leaner patients this target may not be reached. The centrifuged fat is transferred to small syringes in preparation for injection. We prefer 5-10cc syringes. Blunt-tipped 14G x 15cm injection cannulas with single side ports (Coleman Type II) are attached to the syringes for the injection process. Injection is carried out superficially in a fan-like pattern through the same points on the areolar margin (12:00, 3:00, 6:00, 9:00) through which the spinal needles were inserted during TLA infiltration. In most instances, the needle track is sufficient to admit the cannula; if not, a 1-mm dermapunch incision is made. When necessary, additional injections are made along the periphery of the breast margin. The injection cannula is inserted to reach the level of the breast margin marks and fat is injected evenly as the cannula is withdrawn. Typically 1ml of fat is deposited per pass. Large volume deposits are avoided in order to maximize contact with of the transplanted fat with the native recipient tissues. In the event that contour deformities or tissue distortion resist volumetric expansion, tension in the injection planes is released by focal undermining with V-tipped dissection cannulas, disruptor cannulas or microscissors The injection process can be done with the patient supine or with the table flexed and the patient in the semi-recumbent position or they can be alternated as needed to assess the contours as they develop. It should be noted that current techniques of autologous fat transfer to the breast intentionally avoid direct injection into the breast parenchyma. While the injection of the superficial planes usually gives sufficient size enhancement, some surgeons seeking to achieve increased breast mound projection target additional injections into the pectoralis major and the prepectoral layers. Post-Op ManagementAt the conclusion of the procedure, the areolar injection points are covered with steri-strips. Absorbent pads and compression garments are placed over the harvest sites. The breasts are fitted with a tight conforming bra and the patient is discharged home. The patient is seen for follow-up at 24-48 hours post-surgery primarily for surveillance of the harvest sites. Active fluid expression of these areas, if necessary is conducted by the nursing team. The breasts are examined for signs of excess bruising or infection; the latter is rare. Oral broad spectrum antibiotic coverage for skin pathogens is maintained for the first seven days after surgery. Analgesic needs are typically minimal and NSAIDs are usually sufficient. Patients are able comfortably to return to a desk job by 48 hours post-surgery. Additional postoperative surveillance is conducted on a bi-weekly, then monthly basis as deemed appropriate. The final breast volume stabilizes by approximately three months after surgery. ComplicationsDamage to the chest wall is unlikely with autologous fat transfer to the breast because the injection is limited to the superficial plane. Of more concern, but rare, would be infection of the transplanted fat. We have not seen this complication on the breast, but in other areas such as the buttocks, infection of transplanted fat is managed by the expression of the transplanted fat through the sites of injection either manually or with the assistance of liposuction cannulas in conjunction with aggressive antibiotic coverage and may require more than one session. Significant loss of augmented breast volume is common especially in cigarette smokers. The patient needs to be counseled thoroughly prior to surgery that a noticeable portion of the immediate postoperative fill volume represents anesthetic fluid within the breast and fluid within the transplanted fat. Interventions which promote the healing process include adequate caloric intake and smoking cessation, but these no offer no guarantee of superior results. Repeat sessions of autologous fat transfer to the breast should be scheduled at an interval that allows for complete healing and revascularization of the recipient site; typically three months or more. One small case series from Japan, of patients presenting with palpable indurations six months to six years post injection by “untrained individuals” reported pain, infection, breast discharge, lymphadenopathy, and cysts requiring surgical excision (16). They and others have postulated that possible large volume mass injection is a contributing factor to large areas of fat necrosis (16-18). Mammographic changes observed in breasts subjected to autologous fat transfer include various calcifications, cysts, and tissue remodeling in less than half of patients (17). It has been argued that these changes may interfere with breast cancer screening (16, 19), but it has also been argued that the incidence and significance of these findings are no worse than those following other cosmetic breast procedures (4, 20). Furthermore, it has been stated that radiographic multimodal follow-up evaluation is effective at discerning the characteristics of injected fat over time and that no increase in the increase of breast cancer has been reported to date (17, 21). SummaryBreast augmentation with autologous fat transfer is an option for some women seeking a modest increase in size and/or the correction of breast contour deformities. Partial loss of injected volume and the need for multiple treatment sessions are common. The current literature demonstrates low complication rates in experienced hands, mammographic changes distinct from cancer at a rate no higher than that of other cosmetic breast operations, and no apparent effect on the incidence of breast cancer. The use of adjuncts including external tissue expansion, adipose derived stem cells and platelet-rich plasma has not been proven superior, but has not been studied adequately. References1. Cosmetic Surgery National Data Bank. 2008 Statistics. American Society for Aesthetic Plastic Surgery 2009. P. 3.
2. Bircoll MJ. Case report: Cosmetic breast augmentation utilizing autologous fat and liposuction techniques. Plast Reconstr Surg 1987;79:267-71. 3. ASPRS Ad-Hoc Committee on New Procedures. Report on autologous fat transplantation. September 30, 1987. 4. Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: Safety and efficacy. Plast Reconstr Surg 2007; 119:775-85. 5. Gutowski KA. Current applications and safety of autologous fat grafts: A report of the ASPS Fat Graft Task Force. Plast Reconstr Surg 2009;124:272-80. 6. Pelosi MA III, Pelosi MA II. Breast Augmentation. In: Rayburn WF, Laube DW, eds. Cosmetic Procedures in Gynecology. Obstetrics and Gynecology Clinics of North America 2010 December; Vol. 37, No. 4: 533-46. 7. Khoury RK, Schlenz I, Murphy BJ, Baker TJ. Nonsurgical breast enlargement using an external soft-tissue expansion system. Plast Reconstr Surg 2000;105:2500-12. 8. Khoury RK, et al. Brava and autologous fat transfer is a safe and effective breast augmentation alternative: Results of a 6-year, 81-patient, prospective multicenter study. Plast Reconstr Surg 2012;129:1173-87. 9. Mizuno H, Hyakusoku H. Fat grafting to the breast and adipose-derived stem cells: Recent scientific consensus and controversy. Aesthet Surg J 2010;30:381-9. 10. Yoshimura K, et al. Cell-assisted lipotransfer for cosmetic breast augmentation: Supportive use of adipose-derived stem/stromal cells. Aesthet Plast Surg 2008;32:48-55. 11. Fraser JK, Hedrick MH, Cohen SR. Oncologic risks of autologous fat grafting to the breast. Aesthet Surg J 2011;31:68-75. 12. http://www.selphyl.com 13. Eppley BL, Pietrzak WS, Blanton M. Platelet-rich plasma: A review of biology and applications in plastic surgery. Plast Reconstr Surg 2006;118:147e-159e. 14. Salgarello M, Visconti G, Rusciani A. Breast fat grafting with platelet-rich plasma: A comparative clinical study and current state of the art. Plast Reconstr Surg 2011;127:2176-85.) 15. Pelosi MA III, Pelosi MA II. Liposuction. In: Rayburn WF, Laube DW, eds. Cosmetic Procedures in Gynecology. Obstetrics and Gynecology Clinics of North America 2010 December; Vol. 37, No. 4: 507-19. 16. Hyakusoku H, et al. Complications after autologous fat transfer to the breast. Plast Reconstr Surg 2009;123:360-70. 17. Veber M, et al. Radiographic findings after breast augmentation by autologous fat transfer. Plast Reconstr Surg 2011;127:1289-99. 18. Delay E, Garson S, Tousson G, Sinna R. Fat injection to the breast: Technique, results, and indications based on 880 procedures over 10 years. Aesthet Surg J 2009;29:360-76. 19. Spear S, Al-Attar A. Discussion: Mammographic changes after fat transfer to the breast compared with changes after breast reduction. Plast Reconstr Surg 2012;129:1039-41. 20. Rubin JP, et al. Mammographic changes after fat transfer to the breast compared with changes after breast reduction: A blinded study. Plast Reconstr Surg 2012:1029-38. 21. Carvajal J, Patiño JH. Mammographic findings after breast augmentation with autologous fat injection. Aesthet Surg J 2008;28:153-62. Nature abhors a vacuum Preparing a chapter on Cosmetogynecology, I reviewed a mountain of material and reflected on the basic and complex issues that arise repeatedly. One of the very first, and very basic, things which came to mind was the blatant absence of a guide to the terminology of cosmetic gynecology. Even the topic goes by a half-dozen names, some of which you're seeing in these first few sentences. So, without further elaboration, I present you with the first description of the current lexicon of cosmetic vaginal surgery, aesthetic vaginal surgery, female genital cosmetic surgery, or cosmetic female genitoplasty: Preface: Learn a Little GreekThe terms aesthetic, cosmetic, and plastic are related, but they are not synonymous. Grasp this and your ability to articulate your message will improve instantly. Aesthetic derives from the Greek word aisthetikos which means to perceive and judge sensory input as beautiful. When used as an adjective (i.e. an aesthetic contour), it defines the subject as beautiful. When used to describe interventions that enhance beauty, the term is inherently flawed. For instance, the term aesthetic surgery, defines the subject, surgery, as that which is aesthetic, or beautiful. However, the intended meaning of the phrase is something else - that the intention of the surgery is to enhance the aesthetics of he/she who is being operated upon. Not only is this poor grammar, but it also renders any surgery which happens to beautiful to watch, in any field of surgery, as robbed of its proper adjective. Cosmetic derives from the Greek word kosmetikos, which means to adorn or to make beautiful (aesthetic). Here, we have a term that precisely defines the intent to beautify. Cosmetic surgery thus, properly and accurately identifies any surgical process which intends to enhance the aesthetics of the person being operated upon irrespective of whether the surgical process is itself aesthetic. In brief, a cosmetic process creates an aesthetic product, while an aesthetic process creates an undefined product. Plastic derives from the Greek word plastikos, which means to reshape. Plastic is a nonspecific concept that does not define the reason for the action. When applied in the term plastic surgery, further classification is required when specificity is desired (i.e. reconstructive plastic surgery). Adding complexity to the confusion are the observations that plastic surgery is the common name of a surgical specialty with both noncosmetic and cosmetic subdivisions (which some refer to as aesthetic plastic surgery), that many operations in many surgical specialties outside of plastic surgery reshape the body for various reasons, and that surgeons from many specialties provide cosmetic surgery. The Lexicon of Cosmetic Gynecology 2013:Clitoral hood reduction, excision of excess prepuce, or excision of periclitoral labial reduplication, are procedures which target redundant, loose skin at, and around the clitoral prepuce either alone or at the time of labiaplasty. These procedures lack a uniform descriptive term. "Hoodectomy" is a poor terms for these procedures because it implies that clitoral hood proper is being degloved either partially or in its entirety - maneuvers that are not done in the conduct of cosmetic gynecology.
Clitoroplasty refers to surgical alterations in the shape of the clitoris proper, either glans or shaft, done for conditions associated with clitoral hypertrophy rather than for the cosmetic enhancement of normal anatomy. Partial excision is termed clitoral reduction or partial clitoridectomy and is not done for cosmetic reasons. Dermalipectomy is a term frequently used in cosmetic and plastic surgery to describe the en bloc excision of skin and fat. It is usually performed in tandem with the development of a flap of adjacent tissue for the purpose of reducing tissue laxity. Common applications include abdominoplasty, thighpasty, and in cosmetic gynecology, mons pubis "lift" procedures and labia majora volume reductions. Designer laser vaginoplasty™(DLV™) is a term trademarked by Dr. David Matlock’s franchise business which references the entire category of labiaplasty procedures as well as alterations of the loose skin at and near the clitoral hood all performed with laser techniques. Confusion is generated by the inclusion of vaginoplasty in the term despite the fact that it does not reflect the performance of a vaginoplasty in the procedure. Genitoplasty refers to any procedure which reshapes the male or female genitalia. It does not imply cosmetic or therapeutic intentions. Thus, it must be further classified whenever it is used. The most common utilization is feminizing genitoplasty which describes procedures intended to give ambiguous genitalia a female appearance. Hymenoplasty describes procedures designed to create a pseudo hymenal membrane from either existing hymenal tissue or nonhymenal local soft tissue usually with the intent to provoke bleeding at subsequent coitus when the membrane is caused to tear. Synonyms include hymenorrhaphy, hymen reconstruction, and hymen restoration. Revirgination is a poor term because the loss of virginal status is a matter of history, not of anatomy. Labiaplasty or labioplasty, can refer to any procedure which alters the contours of either the labia majora or the labia minora whether it involves reduction, reconstruction or augmentation. Commonly it references labia minora reduction by excision which is the most requested labial alteration. Labial reduction is sometimes used synonymously with labia minora reduction. The most frequently performed labia majora alterations are augmentation by autogolous fat injections and excisional reduction. The more specific terms labia minoraplasty and labia majoraplasty are less frequently used. Laser vaginal rejuvenation™(LVR™) is a term trademarked by Dr. Matlock’s franchise to reflect vaginoplasty procedures performed with laser techniques. Others have taken to using the term vaginal rejuvenation to indicate vaginoplasty with or without the use of lasers. Monsplasty refers to any procedure which alters the contours of the mons pubis. These include liposuction procedures which reduce perceived excess adiposity as well as resections of skin and subcutaneous fat (dermalipectomy) performed alone or in conjunction with abdominoplasty. The use of any technology to assist in the liposuction process such as laser, ultrasound, etc., typically is indicated by use of the technology as a prefix (i.e. laser-assisted, ultrasound-assisted, etc.). Nymphectomy and nymphoplasty are terms synonymous with labia minoraplasty. They are less commonly used in contemporary English literature, but are sometimes used in French (nymphoplastie), and commonly in Spanish (ninfectomia, ninfoplastia), respectively. Vaginoplasty refers to any procedure targeted at reducing the vaginal caliber. These include approximations of the perineal body (perineorrhaphy or perineoplasty), and posterior colporrhaphies with or without plication of the levator muscles. In most cases, both procedures are performed together to produce a longer section of reduced vaginal caliber. This is the complete presentation delivered at Baystate Medical Center, Springfield, Massachusetts, on March 20, 2013. View the references here. View the slides-only YouTube version here. It is the pro stance in a pro-con debate on cosmetic gynecology delivered to an audience of non-cosmetic medical professionals, mostly gynecologists. Beauty is sometimes described as a cultural currency. Nature distributes beauty randomly & this doesn’t sit well with our sense of wanting to treat individuals equally. But this is simply an observation. The Egyptians were great admirers of beauty and left us with a large historical record of their efforts to enhance appearance. The ancient Greeks and the Romans personified their visions of beauty in the statues of their gods. The Greek root of the word “aesthetics” means that which relates to sensory perception. Aesthetics is the application of values and judgments to that which we sense, it’s totally subjective. Beautiful, good, bad, ugly, are applied to anything we perceive. We do this universally. But why do we do this? It is theorized that our thinking processes adapted along with our bodies to ensure survival in the primitive world of the Stone Age. Our brains evolved to do this. The study of this topic is termed evolutionary psychology. It’s a relatively new field, but it is gaining incredible traction among scholars in many disciplines. We're only going cover a few of the relevant aspects of evolutionary psychology as they relate to cosmetic surgery. Evolution favors processes that maximize the reproductive potential of the population as a whole. Individuals who display reproduction-positive thinking processes will be more likely to reproduce & pass on those thinking processes to future populations. Over many generations and hundreds of thousands of years, the majority of individuals in future populations will display these traits. Aesthetic standards of human beauty are an example of an evolved thinking process. These unwavering qualities of human appearance have been deemed beautiful, attractive and desirable in every culture from the beginning of recorded history. These standards have always existed and they are NOT arbitrary. They are a good complexion, symmetrical features, and youth. But why are these the standards...? Because they’re blatant displays of reproductive mate value. They’re not perfect markers by any means, but if you’re back in the primordial savannah of the Stone Age, attraction to young, symmetrical, & smooth-skinned mates gives you the best reproductive odds. Complexion, symmetry, & youth are the universal standards of beauty. Psychologists, anthropologists, sociobiologists and others have studied people from vastly different cultures. All of them have come the same conclusion. Study after study demonstrates consistency in judging beauty. Photographs are shown to people from different cultures yet they all consistently agree on which people are most beautiful. We don’t learn what beauty is, we know what beauty is…and it’s not in the eye of the beholder... This startling revelation has been documented consistently in psychological studies using photographs of faces judged attractive by adults. One study demonstrated this in 3-to-6 month-olds. Another study, by one of the giants in this field, Judith Langlois, showed it in 2-to-6 month-olds. A study in the late 1990s showed this tendency in newborns less than one week old. One week old babies have standards of beauty. And it’s the nature of both sexes. Male or female, it’s seems unnatural to be attracted to anything else. Let’s discuss the relationship between standards of beauty, which are natural, and the media, which is man-made. Is the media really creating unhealthy stereotypes that otherwise wouldn’t exist? Does the media really decide what beauty is? If we suppose that advertising defines beauty, then we have to presuppose that complexion, symmetry and youth have no intrinsic attraction to begin with. Does anybody really believe that? Newborn infants don’t believe that. Stone Age man didn’t believe that. The ancient Egyptians didn’t believe that. And marketing firms don’t believe that either. So what’s their angle? They hope that your attraction to complexion, symmetry & youth will spill over onto their product if it’s attached to it... Thank Dr. Pavlov and his dogs for the concept. Advertising is all about getting attention. Catering to our natural attractions has always been the solid bet. The problem with the media is perceptual contrast. What that means is that to outcompete each other for attention, competitors need to use increasingly attractive people to succeed. If you overexpose yourself to the media you might develop a distorted sense of what constitutes an average level of attractiveness, but you’re still attracted to complexion, symmetry and youth. Portable technology attached to media distribution networks overexposes us to the media if we overuse it. The Greek origin of the word “cosmetic” means to adorn or to make beautiful. Cosmetic relates to the process of enhancing something to make it more aesthetic. The term aesthetic surgery is a misnomer – what it really implies is that the surgery itself, like a ballet is beautiful to watch regardless of what’s being done. It has no reference to intent. Plastic means simply to reshape. It too, is without reference to the intent of the reshaping effort. If we use language precisely, then cosmetic surgery is the only term that appropriately defines surgery done with the intent to enhance aesthetics. Like advertising, cosmetic medicine, surgery and products promote complexion, symmetry and youth. But they promote it as something that you can participate in. As a global culture, we don’t just accept cosmetic surgery & medicine. We celebrate it and we participate in it…because it aligns with our attraction to complexion, symmetry and youth. Just like the mirror in your purse, like the braces on your teeth, like the paint on your hair. There has never been a shortage of opinion on cosmetic surgery, but in every culture that has ever existed people have willingly availed themselves of the methods and technologies available at that time to pursue enhanced complexion, symmetry and youth. Some people don’t like cosmetic surgery, and they don’t like that other people like cosmetic surgery. And they don’t like that people do cosmetic surgery, but since our culture tolerates cosmetic surgery they try to attach cosmetic surgery to things that people don’t like to try to convince people to think like they do. They claim that cosmetic surgery is equivalent to false advertising. Nobody likes false advertising. Sure, there are plenty of examples of false advertising in cosmetic surgery, in non-cosmetic surgery, and in every industry that advertises, but that’s a judgment on advertising, not on the merits of surgery itself. Some say that cosmetic surgery is porn-driven. It’s not. Porn is media. They want to display complexion, symmetry and youth to sell their product just like any other type of media. It’s another example of advertising promoting universal innate standards. If porn were the global arbiter of style, then we could also make the case that leanness, bleached hair, overdone lips, breast implants and fake orgasms are porn driven too. Don’t try to argue that pornography has ever set standards of beauty. Porn is simply another messenger of the innate message of complexion, symmetry and youth. Some people allege that since their elders didn’t discuss cosmetic surgery, that it’s a new fad. Today’s Baby Boomers went through puberty in the 1950s. The parents of that generation were raised to consider many desires as things to remain unspoken & technology didn’t permit any outlet for information or access to products and services that exist today so that argument doesn’t hold up well at all to scrutiny. Mom’s generation and Stone Age man would have behaved identically to today’s generation if they had access to our knowledge and technology. Let's explore the aesthetics of cosmetic gynecology in the light of what we know about human nature. Despite the obvious fact that the genital area requires effort to make it viewable, and that not everyone chooses it to make it viewable, those who do view it from an aesthetic angle apply the same standards of beauty we are all born with. When they view the genital area through the lens of complexion, symmetry and youth, they will develop an opinion. Whatever that opinion is, they may choose to express that opinion by leaving nature alone, by decorating it, or by altering it with or without the aid of a surgeon. If your opinion becomes your obsession you’ll need the services of a psychiatrist. If not, you might visit someone like me. This thought process applies to any part of the body. Anyone who provides cosmetic services will tell you that the key to a successful outcome is in setting a realistic expectation. Cosmetic expectations are unique to the individual & they can’t be measured like treatment outcomes because they are opinions. You can perform identical cosmetic surgeries on identical twins with perfect healing, but the one who expected something else will not be happy. That being said, public displays of some body parts are more ubiquitous than others so that there is a greater general awareness of the variety that exists in any dimension of a given part that is more widely displayed. Thankfully, displays such as "The Great Wall of Vagina," by artist Jamie McCartney, are permitting previously difficult- to-view areas become more publicly viewable. Clearly, this allows for more robust opinions and therefore better decision making. Most of the anti- cosmetic vaginal surgery noise comes from Great Britain. A small group of critics gets quoted widely. Their real gripe is that their socialized medicine National Health Service is getting stuck with the bill for cosmetic vaginal procedures under the guise of bogus medical indications. Australia and New Zealand have similar socialized healthcare & they mimic the British critics. It’s about limited money better spent elsewhere. I would agree wholeheartedly that the cost of cosmetic surgery should come out of the patient’s pocket, but everything else they claim is poorly argued & unsubstantiated. Cosmetic gynecology is a group of procedures. The efficacy of any procedure is completely dependent on what is expected to happen via the procedure. These procedures share the features of many existing procedures in therapeutic gynecology & the risk profile should be similar provided the surgeon has experience in the relevant therapeutic operations. There is no single component of any cosmetic gynecology procedure that doesn't already exist in therapeutic gynecologic surgery. These are general categories of cosmetic vaginal surgery in my current practice. Cosmetic vaginal surgery is not intended to produce or enhance orgasms. Some say that a gaping vagina isn’t a problem if it lacks pain, bowel dysfunction, or urinary dysfunction. They dismiss the importance of vaginal sensation as something that benefits only the male partner & that women could care less. This might apply to some women, but it doesn’t apply to many, many others. But if you don’t ask them, they won’t tell you. The concept of tightening the vagina to enhance sex is over 1,000 years old. The book, Treatments for Women, part of a popular medieval ensemble of books known as the Trotula was written by a woman in Salerno, Italy in 1050 AD. It lists 5 recipes for tightening the vagina with constrictive agents. Arnold Kegel wrote extensively of vaginal laxity and sex. He didn’t think that vaginal laxity was a bogus, male-oriented concern. Increasing vaginal sensation, or coital grasp, is not the same thing as producing or augmenting an orgasm, but that doesn’t mean that some women don’t enjoy improving their sensation, Especially if it has decreased greatly over time. I had a vaginal delivery, kegels don’t work, I don’t have any of the problems on your pelvic floor checklist & I’m healthy. Is there anything you can do? A woman may have a tight vagina, a gaping vagina, or anything in between, but this is the most common story I hear. I saw a patient in consultation yesterday who was belittled and dismissed by a “pelvic floor surgeon” for raising these concerns & it’s not the first time. Thanks to a general misunderstanding of somebody’s Committee Opinion, many gyns are uncomfortable treating this woman further and even hesitate to inquire about the sex life of their established patients – don’t ask, don’t tell, or go to hell. They’ll either send her my way or tell her nothing can be done. Sad, but true. I hear these stories all the time. In my practice, this patient gets a full pelvic floor evaluation which every gynecologist should know how to do and her kegel technique gets checked for adequacy. That's the starting point. The method of a vaginoplasty is to tighten the caliber of the lower or distal vagina via posterior colporrhaphy and perineorrhaphy. This can only be done effectively if the pelvic floor suspension is relatively intact and the endpoint is defined. This can only be done effectively if the amount of tightening is measured with precision. If not you’ll need to repair the pelvic floor a preliminary step. If you skip the pelvic floor repairs, the existing floor damage might get worse or your tightening procedure might fail. The bottom line: don’t do vaginoplasties if you’re unfamiliar with these types of repairs unless you get someone experienced in these procedures to help you. The procedures don't fail in achieving the goals they are designed to accomplish. Failure is in choosing the wrong procedure for the wrong reasons. Labiaplasty is performed for various reasons, it’s not always bilateral, it’s not always excisional, and the anatomy varies widely. If we’re going to discuss labiaplasty we need to keep these things in mind. Especially since the procedure may involve just a little bit of surgery or something more involved. Also, labiaplasty is not a new operation, and neither is "cosmetic" a new indication. The first labiaplasties were done in seventh century AD for aesthetic reasons as well as for symptomatic ones, but not necessarily for both together. This knowledge has been widely available for over three hundred years. The British opponents of cosmetic vaginal surgery have attempted to extrapolate the complications of extensive surgery performed on newborns in the 1970s by techniques abandoned in the 1980s as potential complications of cosmetic labiaplasty on normally developed adult women. All of these troublesome effects of intersex surgery are related to nerve damage associated with partial amputation of the clitoris, folding of the clitoral shaft, or with the creation of false labia from surrounding tissue. None of this bears any similarity to cosmetic labiaplasty nor to cosmetic alterations of the loose skin around the clitoral hood which do not impinge upon the clitoral nerve supply. I don’t like the way they protrude. They don’t cause any discomfort whatsoever... This is a pure cosmetic request. Her request is not about sexual function. She needs to understand that, you need to understand that. The intent of cosmetic labiaplasty is to achieve the anatomic endpoint requested by the patient. If the request or expectations are unrealistic, the intent will not be realized. They bother me... This is either a pure cosmetic request in disguise or a valid complaint. Evaluation for causes of vulvar pain is the first step. Sadly, if labiaplasty is required many physicians and all insurance companies will deny the request. There is a misconception among gynecologists and other surgeons that labiaplasty is a quick and easy procedure. They believe that the procedure consists of a crude amputation with oversewing of the labial edge. It is true that butchery of that sort can be accomplished quickly. But that is not cosmetic labiaplasty, that is labial amputation & it will never yield satisfactory aesthetic results. Sadly, I've seen the technique used on documentaries painting labialplasty in a negative light. A real cosmetic labiaplasty takes thoughtful aesthetic planning, anatomic caution, and meticulous technique. This takes time, patience and skill. It's not a coincidence that those who perform a large volume of cosmetic labiaplasties take their time. Another poorly constructed argument by the British opponents of cosmetic labiaplasty postulates that since labia vary greatly in dimensions and patients requesting cosmetic labiaplasty fall generally within the normal range of measurements, they shouldn't be permitted to alter these dimensions. Not only is this argument absurd & inconsistent when one considers that the majority of all cosmetic requests on any part of the body involve structures which fall within the normal range of dimensions, but it completely misses the point that those who request cosmetic alterations wish to be in a specific ideal range within the normal range. It's hypocritical & patriarchal when these small groups with extreme ideas intolerantly criticize those who have a differing opinion on cosmetic surgery and they remain silent on parallel procedures performed performed upon males or upon other body parts. The topics of monsplasty (liposuction and/or surgical lifting & tightening) and hymenplasty were listed, but not discussed due to time constraints. Those who are unfamiliar with cosmetic surgery fees claim that prices seem high. Their basis for comparison might be the low frequently undervalued reimbursement rates that they accept for their work from third-party payers for therapeutic medical services. But cosmetics is not therapeutics. It's a luxury service. In fact, taking similarities in operating time and requisite resources into consideration, cosmetic vaginal surgery fees are in the same range as most breast augmentation and liposuction procedures, and less than those typical of abdominoplasty, face lifts, and cosmetic dentistry. No talk about cosmetic gynecology would be complete without talking about David Matlock. David started out practicing Ob Gyn in Beverly Hills in the 1980s. He started offering vaginoplasties to enhance sex in a newspaper ad after a few patients who underwent colporrhaphies for gyn conditions mentioned that it had a positive effect on sex. He went to business school several years later and made this the focal point of a business school project. He trademarked his style of vaginoplasty and labiaplasty, then added the G-shot for the G-spot to round out his portfolio of cosmetic gyn services. Then he developed a franchise model for others to learn the procedures and perform the procedures using trademarked terminology. But what really departed from anything that had been done by anyone in medicine before was that he instituted a gag clause. He started this business in 2002 with heavy advertising in journals and then at meetings. Around the same time, cosmetic surgery exploded in popularity worldwide thanks to the introduction of botox, reality tv, a lax credit market and the birth of social media. Cosmetic gyn was all over the media even though in reality, the number of cosmetic gyn surgeries, even in David’s clinic didn’t approach the number of procedures performed for breast augmentation or liposuction in busy cosmetic practices including his own. Nonetheless, in 2007, ACOG, for the first time addressed cosmetic vaginal procedures by means of a Committee Opinion from the Committee on Gynecologic Practice targeted directly at David’s business. The committee which produced the opinion defines itself as a developer of state-of-the-art commentaries. The ACOG Committee on Gynecologic Practice produced 3 Opinions in 2007. As you would expect, they normally support their state-of-art opinions with references. As you can see, the first two had a total of 22 references combined, but this opinion only had one reference. They carefully crafted their document to identify all of Matlock's trademarked terminology without infringing upon the trademarks and incurring legal exposure. They stated that his terminology was unclear, they speculated as to what they thought the procedures might be, they speculated as to what they thought the complications might be based on their unreferenced assumptions, they filled it with innuendo. But most importantly, what they didn’t do was interview David. The ACOG motive for issuing an alarmist document lacking even the most basic review of relevant literature is unclear, but it does not appear that the motive was to produce a state-of-the-art commentary. It only has one reference. And what was this incredible reference... A paper that states that vulvar and vaginal dimensions vary. That’s it! Strangely enough, just one year later a non-physician from New Zealand submits a review article on cosmetic gyn and finds over 150 references many of which predated the ACOG opinion. The merit of this document needs to be understood for the piece of political propaganda that it represents. It has stood unchallenged long enough and it has never been a state-of-the-commentary on cosmetic vaginal surgery. I’m done talking about David & stirring up the pot. We need to stop ignoring people who request cosmetic gynecology services. We need to stop dismissing their concerns as trivial. We need to accept that there is nothing wrong with cosmetic surgery. We need to give realistic expectations of what cosmetic surgery can and cannot accomplish. END OF LECTURE Author's NoteI ended the lecture three slides short of the planned ending due to time constraints. The real ending was intended to evoke a strong and uncomfortable emotional response among audience members by challenging root values and the meaning of ethics. Think about them as the provider of the service, the choices you make & that society must make to justify the actions. Here are the slides:
Vaginal rejuvenation, or tightening, is over one thousand years old, and it was conceived by women. As mentioned in Part I, the work of the female physician Trotula de Ruggiero of Salerno was published in 1050 AD under the title Treatments for Women. In this volume are five nonsurgical recipes for "restoring" virginity. The section opens as follows: A constrictive for the vagina, so that women may be found to be as though they were virgins, is made in this manner Renowned Medieval historian Monica Green who spent decades researching all extant versions of the Trotula ensemble and Salernan culture prior to her definitive translation opines: It may be that some of these constrictives were meant only to tighten the vagina to the enhance the friction of vaginal intercourse, not necessarily to produce a fake bloodflow of "defloration"; in other words, they may have been intended as aids to sexual pleasure within marriage. The Renaissance brought major advances in anatomic knowledge through cadaveric dissections best represented by Vesalius (1514-1564) at the University of Padua in De Humana Corporis Fabrica. Owing to the invention of the printing press, this knowledge became widely disseminated. However, little if any change in took place in gynecologic surgical technique or instrumentation from that of the Greco-Roman era . Nonetheless, celebrated French surgeon Ambroise Paré (1510-1590) in Gynaeciorium Physicus et Chirurgicus, then his pupil Jacques Guillemeau (1550-1612) in his 1609 text De la Grossesse et Accouchement des Femmes, were first to describe repairs of rectovaginal lacerations at childbirth. Spaniard Roderico a Castro (1546-1627) described clitoridectomy by a horse hair ligature tightened daily in Philosophiae Ac Medicinae Doctoris per Europum notissimi first published in 1604. The first illustration of excision for clitoral hypertrophy was provided by the German surgeon Johann Schultes (aka Scultetus 1595-1645) in Armamentarium Chirurgicum published posthumously in 1655. Pierre Dionis, a Parisian surgeon, described excision of the nymphae (labiaplasty) in his Cours d’opérations de chirurgie (1707) based on his work in the late 1600s in the court of Louis XIV. German military surgeon Lorenz Heister (1683-1758) described labia minoraplasty in full detail in his text, Institutiones Chirurgicae (1739), one of the most popular illustrated surgical texts of the eighteenth century: The nymphae in women are sometimes so large, as not only to hang without the labia pudenda, but also to prove troublesome to them in walking, sitting, and in their conjugal embraces; and may therefore require the surgeon’s assistance. The operator is therefore in the first place to lay the patient in a proper posture, and taking hold of the nymphae with his left hand, he is then to cut off so much of them with a pair of scissors in his right, as he shall judge necessary, taking care to have in readiness styptics for the haemorrhage, and medicines to prevent the patient from fainting. When the operation is over, the wound may be dressed with some vulnerary balsam, and healed without much difficulty in the common method. Key Points1. Vaginal rejuvenation, or tightening, is over one thousand years old, and it was conceived by women.
2. Clitoroplasty, in the Western world, was performed for appearance only through the eighteenth century. 3. Labiaplasty was an established treatment for both symptomatic and aesthetic concerns by the late seventeenth century. I can think of no finer way to inaugurate the ISCG Blog than to explore the history of cosmetic vaginal surgery. Where possible I have linked to online translations for reference and scholarship. Soranus of Ephesus, a Greek physician who practiced in Alexandria and later in Rome from the end of the first century to the beginning of the second century AD, provided the first written record of surgery performed on the female genitalia for cosmetic effect. In a 6th century Latin translation by Muscio of his 4-volume treatise entitled Gynaecology, he describes the excision of a hypertrophied clitoris for cosmetic reasons and to diminish excessive sexual stimulation. He credits the procedure to Philumenus (not the 3rd century Philumenos), one of his older Greek contemporaries: The patient was placed in a lithotomy position and held in place by able bodied assistants. The surgeon grasped the clitoris with broad toothed forceps and cut above the instrument...Bleeding was controlled by cold compresses soaked in vinegar and styptic powder. Philumenos of Alexandria, in the third century AD, described excision of the hypertrophied clitoris because it was considered "ugly and disgraceful." His work was abstracted by the Byzantine physician Aetios of Amida in his 4th century work Sixteen Books on Medicine. The practice of excising the nonhypertrophied clitoris originated in Egypt in an effort to prevent any desire for coitus in premarital girls and not out of any cosmetic motivation. In the seventh century AD, Paulos of Aegina, another Byzantine physician describes two distinct operations in his Medical Compendium in Seven Books. The first operation is his technique of excision of the hypertrophied clitoris, which he refers to as the nympha. The second operation is an excision of enlarged labia minora which he refers to as cauda pudendi or pudendal tail: The cauda is a fleshy excrescence arising from the mouth of the womb, and filling the female pudendum, sometimes even projecting externally like a tail; and it may be removed in the same manner as the nympha. The suturing of vaginal lacerations at childbirth forms the basis for all modern vaginoplasty techniques. The procedure was first described circa 1050 AD by a female physician, Trotula di Ruggiero of La Scuola Medica Salernitana, the first medical school in Europe. She wrote Treatments for Women as well as contributions to another work De Ornatu Mulierum (Women's Cosmetics) which, in addition to two other works written subsequently by other medieval physicians comprised the compendium commonly known as The Trotula. Key Points1. Cosmetic vaginal surgery can be traced back to the Greek physician Soranus of Ephesus, in first century AD.
2. Labiaplasty was first performed by the Greek physician Paulos of Aegina, in the seventh century AD. 3. The origins of vaginoplasty began with the female physician Trotula di Ruggiero of Salerno, in the 11th century. |
AuthorMarco A. Pelosi, III, MD, is a cosmetic gynecologist, surgeon, lecturer & cofounder of the ISCG. You may contact him directly at [email protected] Archives
April 2020
Categories
All
|
We are ISCG |
Get to Know Us |
Stay Connected |




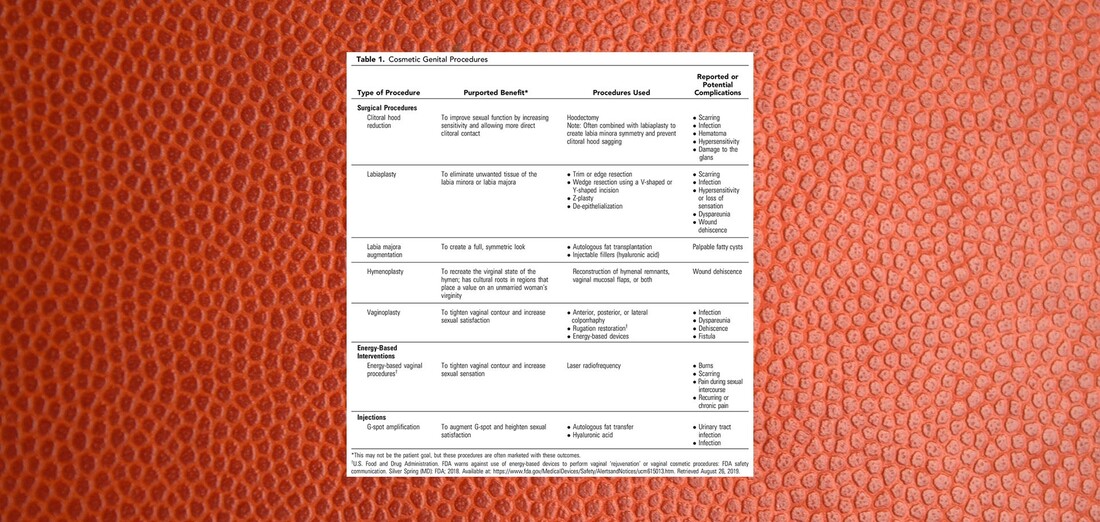

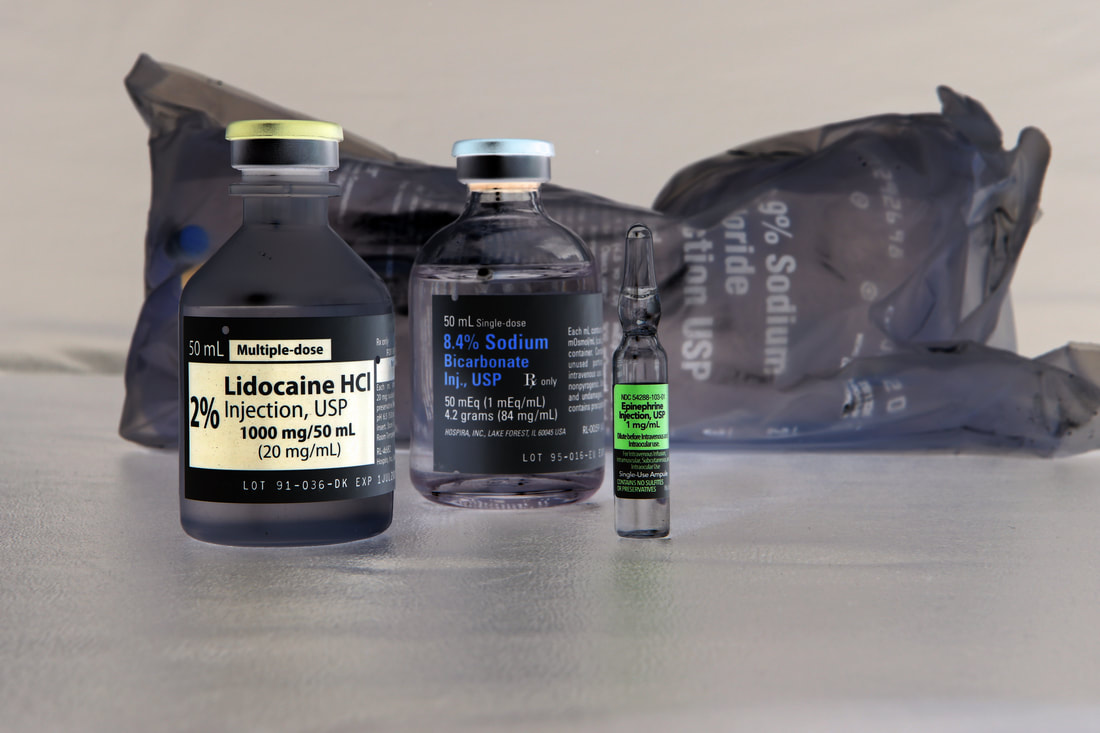




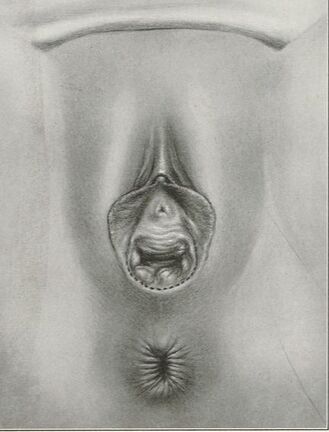
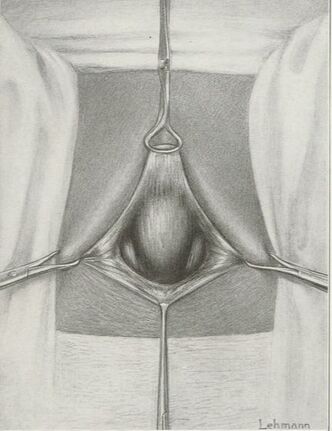
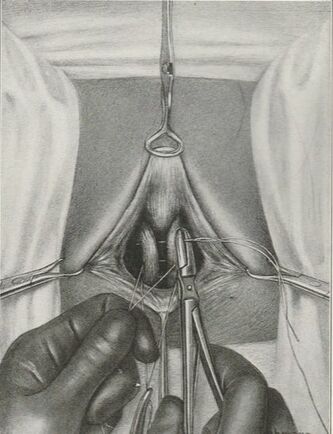
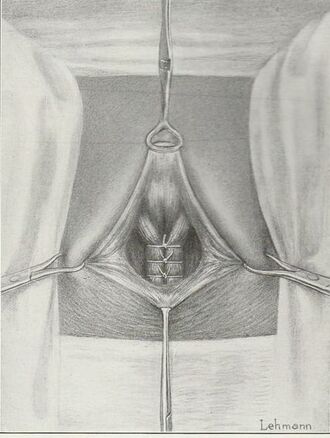
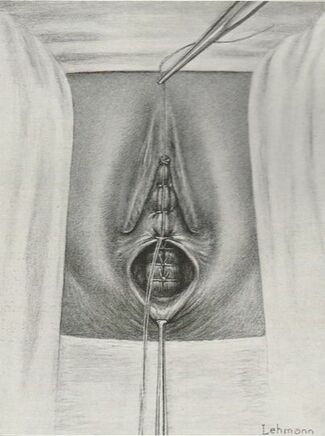
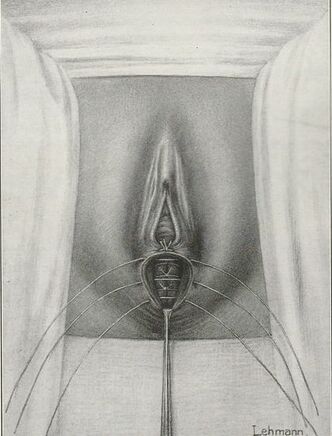
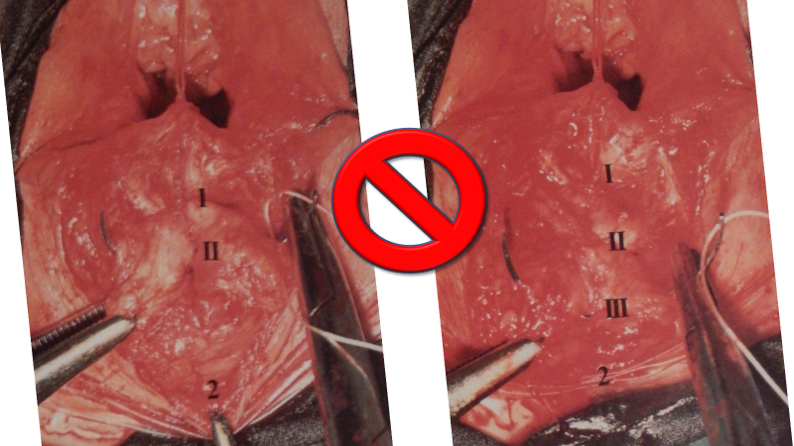






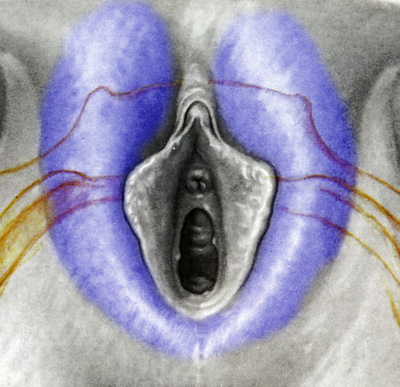
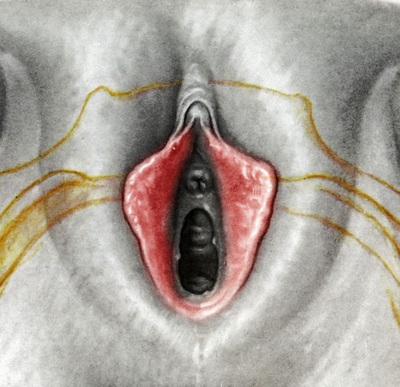



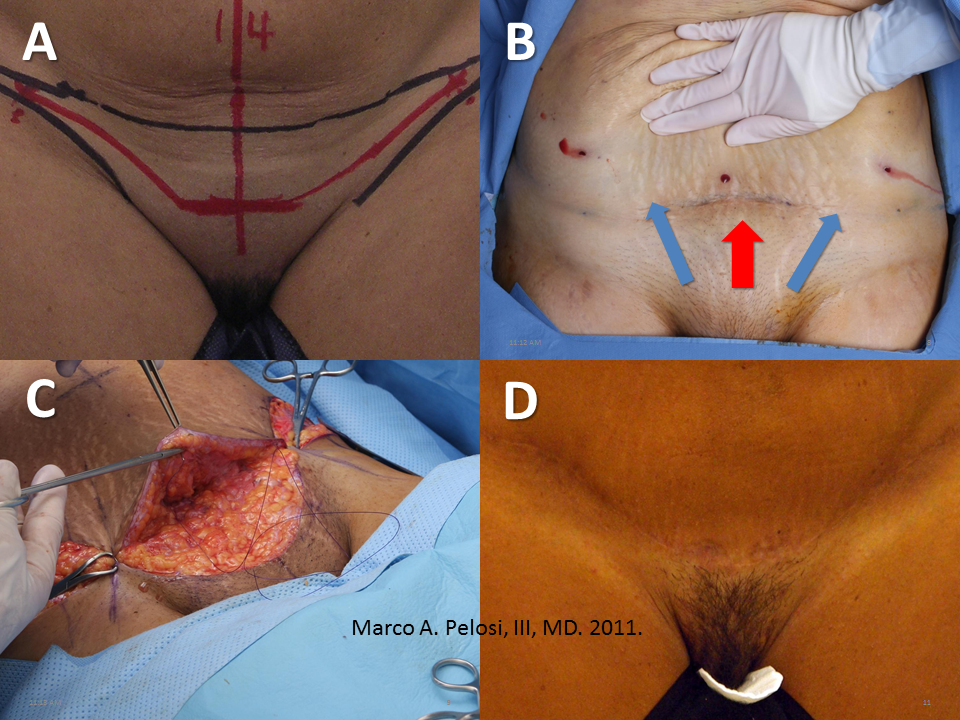

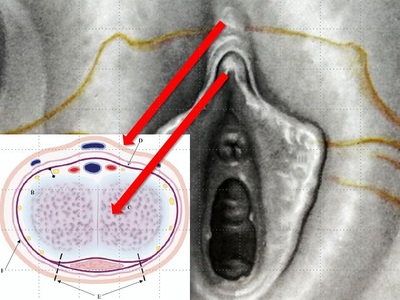

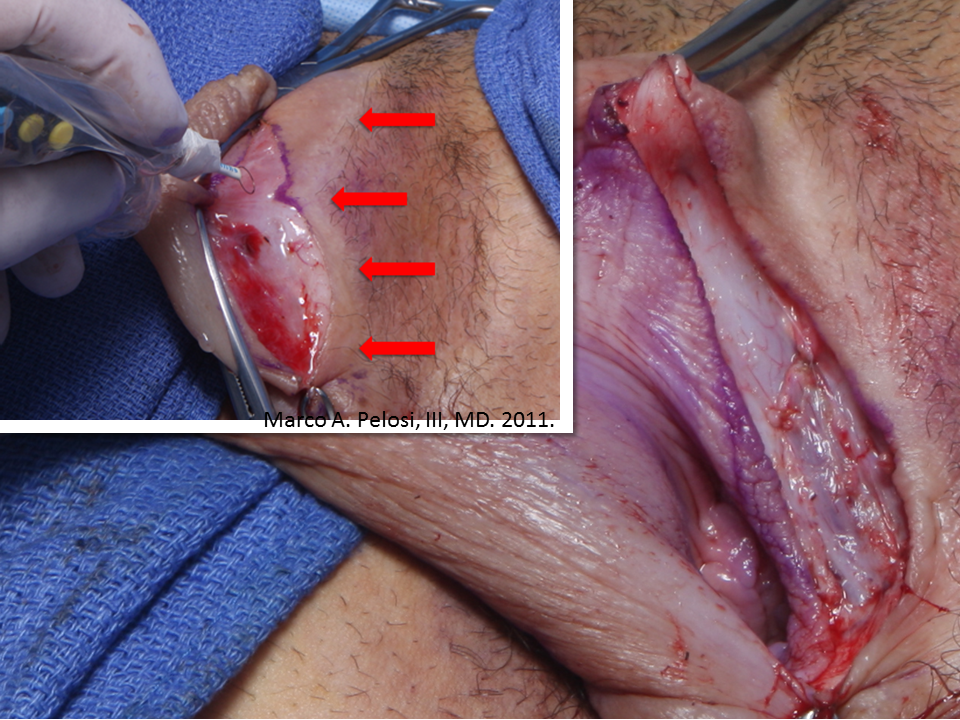
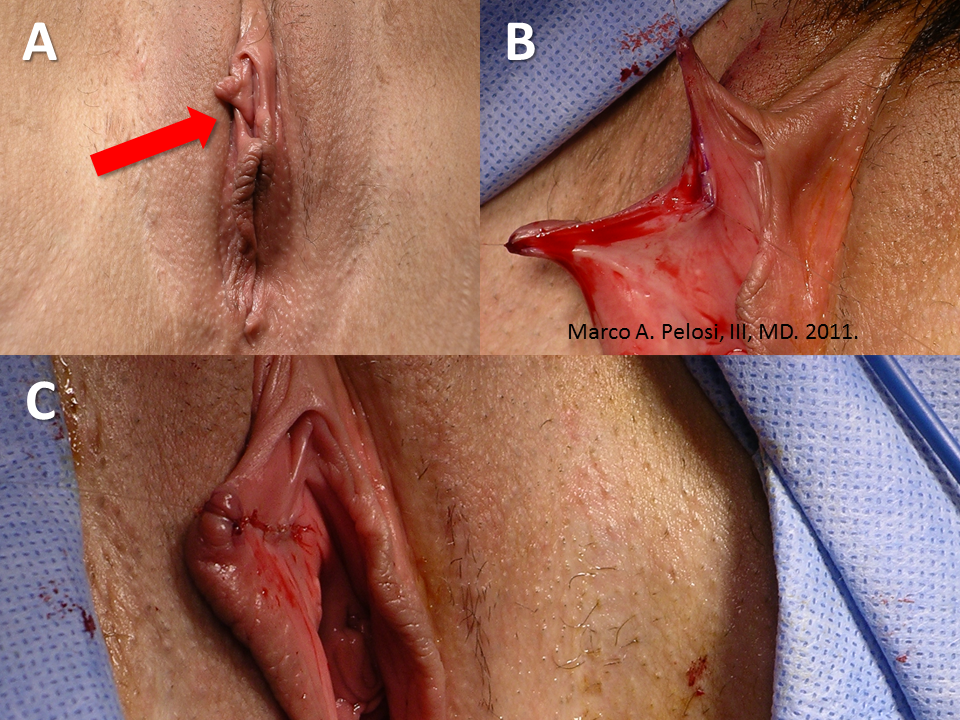
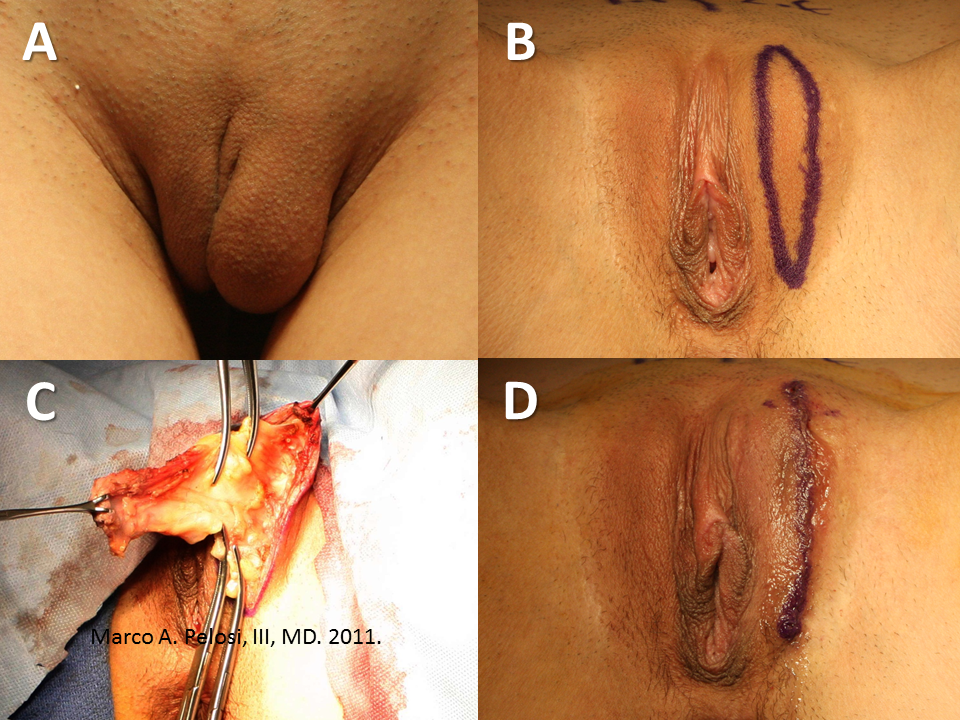
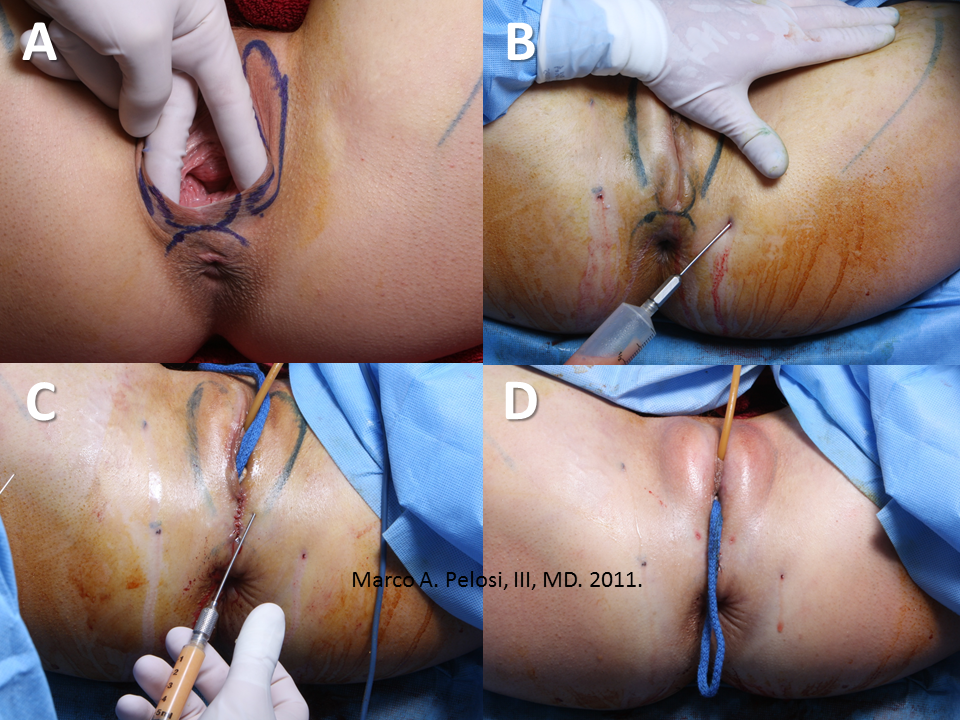








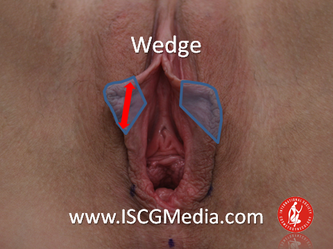

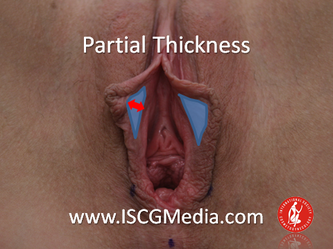
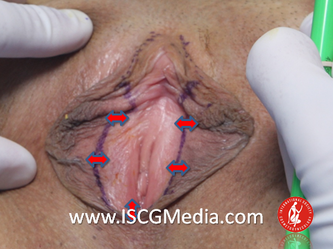






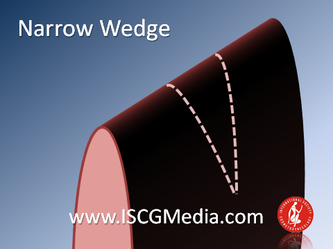
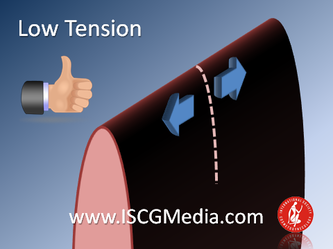
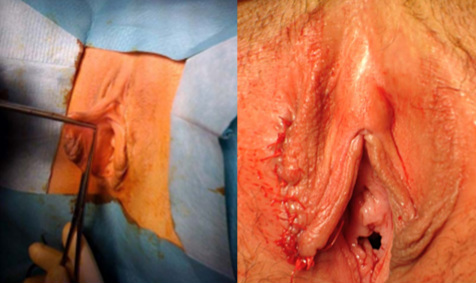
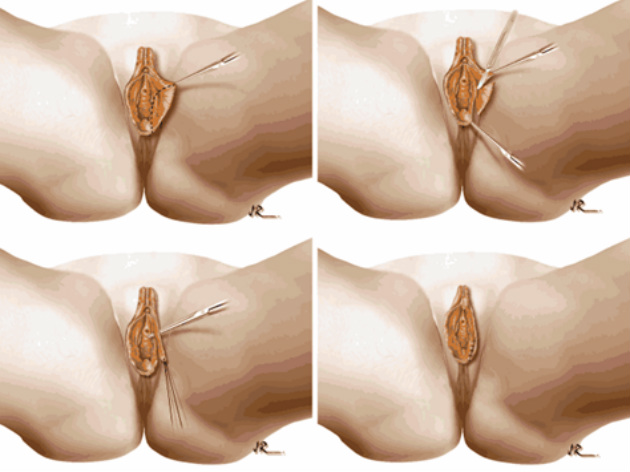
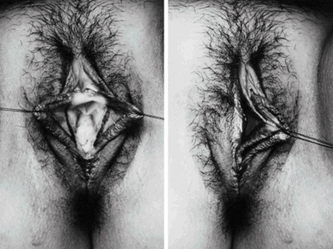
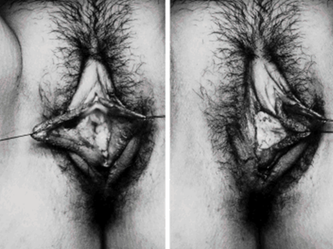


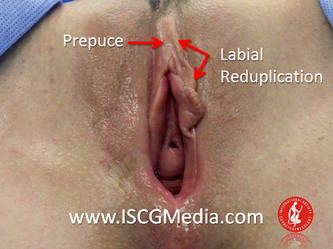
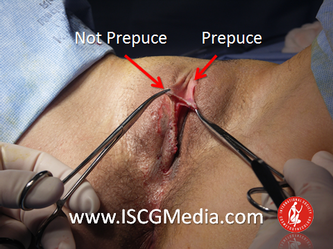


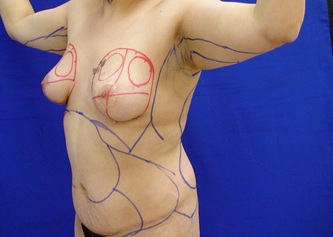





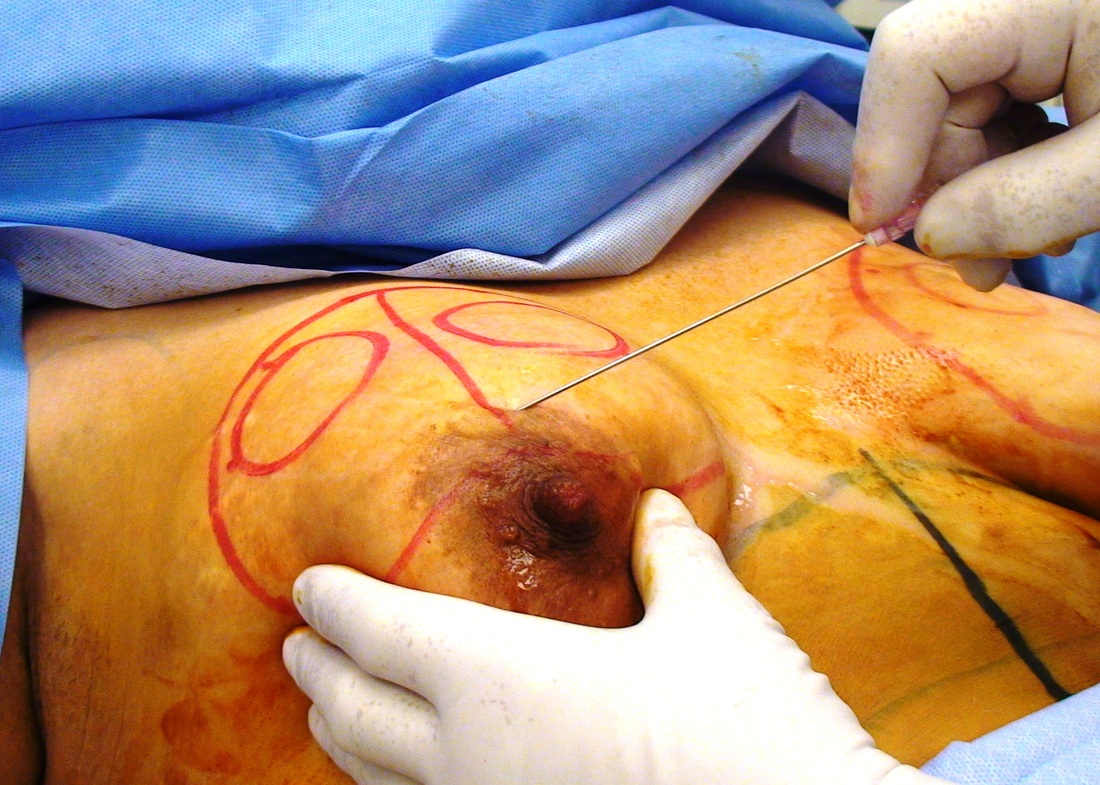







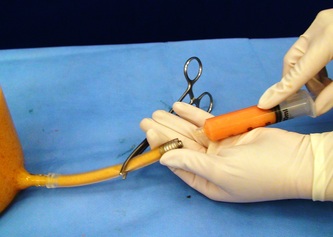
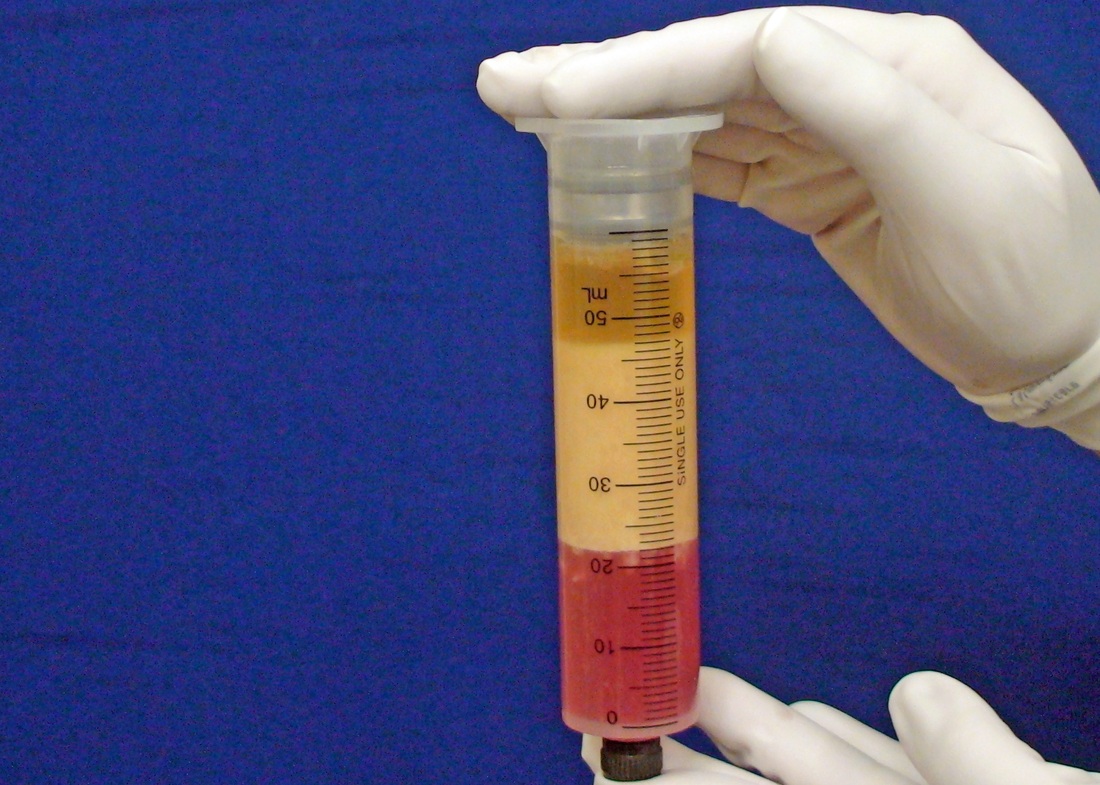

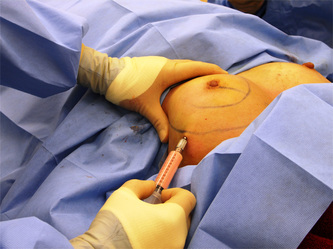

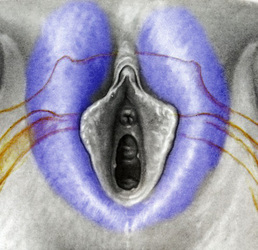








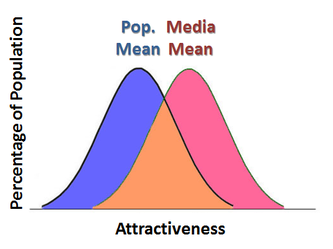







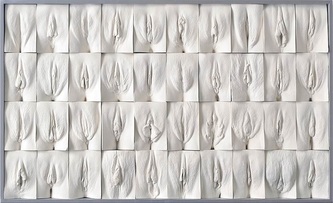
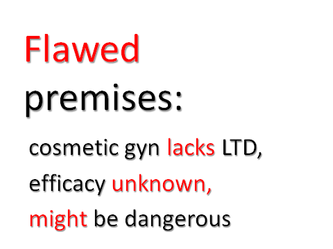
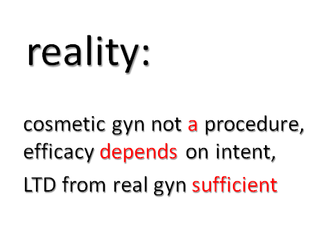
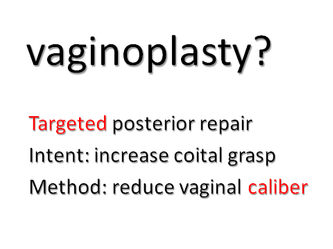

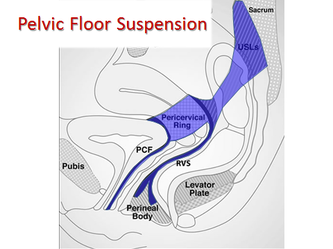
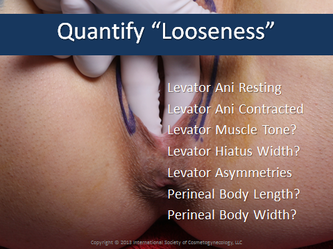
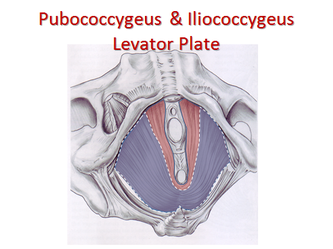
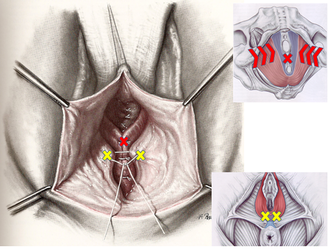
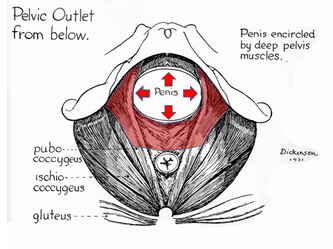
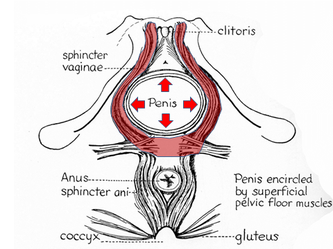

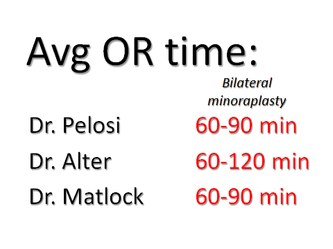
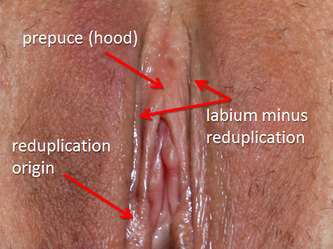
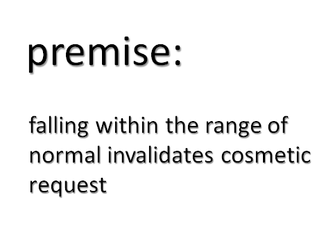
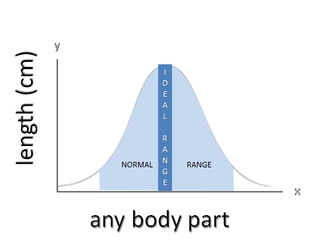




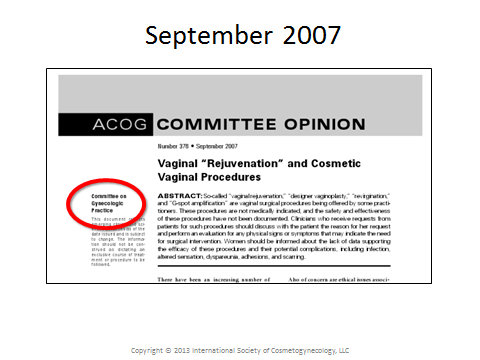
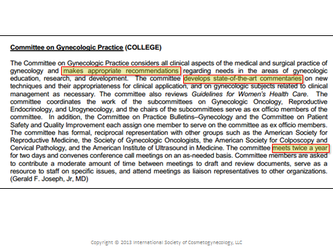
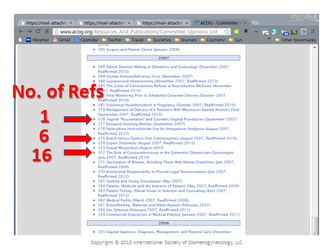
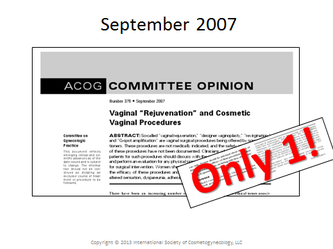
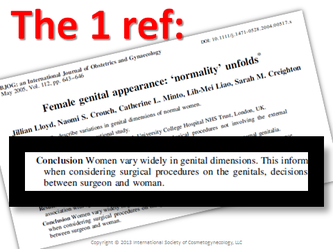

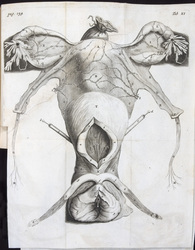

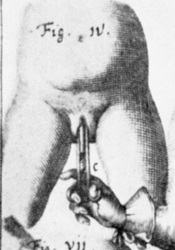







 RSS Feed
RSS Feed
